Now and then, you may have come across the term ‘piles’ but it’s a topic that you usually don’t want to discuss with your loved ones. It often doesn’t cause any major obstacles, however, if they do cause any bleeding or unpleasant pain, it’s time to seek proper medical care. Many people have piles but the symptoms are not always obvious. They are most common among adults aged 45 to 65 but this does not mean that young people and children cannot get them. Women are more likely to get them during pregnancy. Let us now dig deeper into getting a better understanding of piles, its symptoms and treatment options available.
What is Piles?
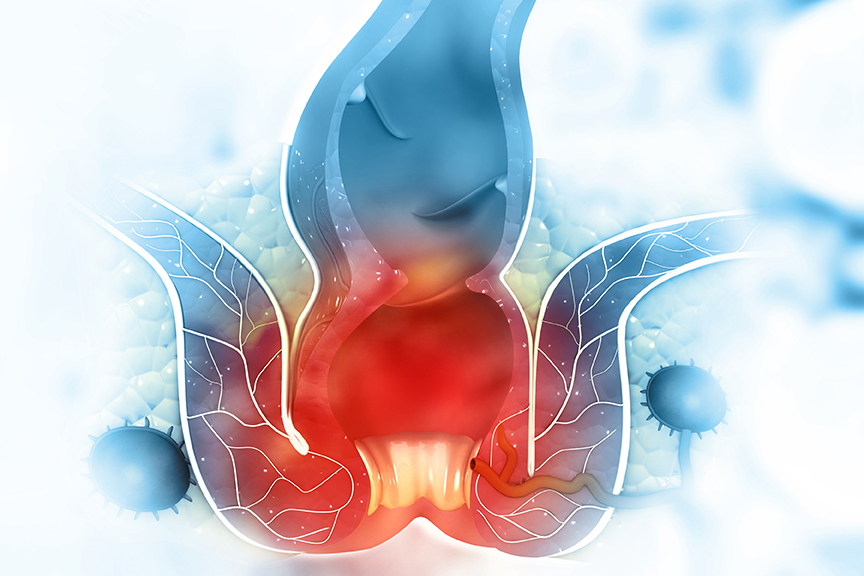
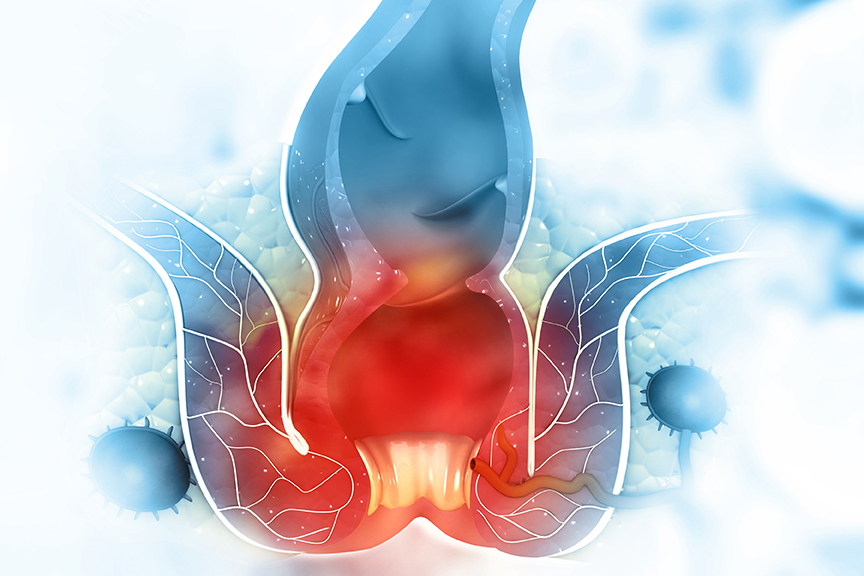
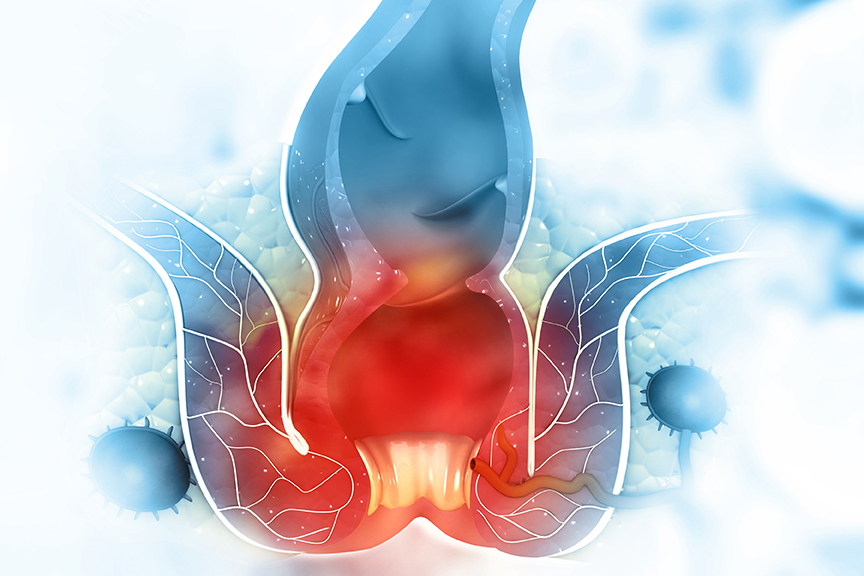
Piles are inflammation of tissues in the anal pathway (canal through which we pass stools). They are a collection of blood vessels, tissues, muscles or fiber. In simple words, they are lumps inside and around your bottom (anus). The size of piles can differ from person to person, and they may be internal or external. Internal piles are usually in the range of 2 cm – 4 cm above the opening of the anus, whereas external piles appear on the outside boundaries of the anus. In some rare cases, people may develop external and internal piles at the same time. Piles are also categorized by their size and severity.
What are the signs and symptoms of Piles?
Small internal piles are normally innocuous. However, larger piles may cause mucous discharge, soreness, irritability, and itch. The most common sign of piles is bleeding post passing stools. Sometimes there are no symptoms at all and you may not even realize that you have one. Nonetheless, a piles patient may experience:
- A hard and painful mass which is present around the anus.
- Feeling of bowels being full, even after passing of stools.
- Noticing bright red blood after passing stools, on the toilet paper or toilet pan.
- Itching and inflammation of the anal area.
- Pain while passing stools.



More severe symptoms of piles include:
- Excessive bleeding from the anus.
- Possibilities of severe infection.
- Inability to control stool passage.
- Anal Fistula (a small tunnel that develops between the end of the bowel and the skin near the anus).
- Strangulation where the blood flow stops in the piles causing infection and even formation of a blood clot.
What are the causes of Piles?
Piles are caused due to the increase of pressure in the lower portion of the rectum. Due to increase in pressure, the blood vessels surrounding the back passage (anus and rectum) get stretched, get swollen or form a lump, which is referred to as piles. Also, some are tend to develop for no apparent cause but there are specific circumstances that may certainly increase the chances of one developing piles such as:
- Long term constipation leading to straining during a bowel movement or prolonged sitting in the toilet. Passing large stools increase the tension in and around the veins.
- Long term diarrhoea/Chronic diarrhoea; Sitting on the toilet pot for too long can weaken pelvic muscles and increase pressure on you rectum and anus.
- Frequent lifting of heavy objects – Straining and holding your breath while lifting weights could cause the veins near your anus to become swollen and possibly push through your anus, resulting in the disease.
- Pregnancy – Piles are common during pregnancy. This is apparently due to pressure impacts of the baby lying above the rectum and anus, and also the effect that the change in hormones during pregnancy can have on the veins. However, this occurrence during the pregnancy often go away after the birth of the child.
- Being obese – Being overweight increases the risks of developing piles.
- Unnatural sexual intercourse.
- Regular consumption of diet poor in fibre content.
- Cancer in the colon – Some symptoms may include bleeding from the bottom, itching, and pain around the anus.
- Prior surgery in the rectum area.
- Injury in the spinal cord.
Your physician can normally detect piles after carrying out a physical checkup. They will check the anus of the person with suspected piles. The session will then be followed up with questions related to your medical history. In the case of internal piles, a digital rectal examination (DRE) or the use of a proctoscope (an instrument used to examine the anal cavity, rectum, or sigmoid colon) is required. A colonoscopy (an exam used to detect changes or abnormalities in the large intestine and rectum) may also be recommended if symptoms of the patient indicate some other digestive disease.
While piles can be hurting and weakening, they do not pose any ongoing threat to health and can be self-managed up to an extent. However, if the complications are serious and causing unpleasant pain and hindrances in your day to day activities, then proper and immediate medical attention is suggested.