The knee is the human body’s largest joint and its healthy maintenance is required to perform most of the everyday activities, easily. The knee joint is formed by the thighbone’s (femur’s) lower portion, the shinbone’s (tibia’s) upper portion, and the cap of the knee referred to as the patella. The ends of these three bones where they meet are covered with a smooth substance that protects the bones and enables them to move easily (articular cartilage). The C-shaped wedges present between the thighbone and the shinbone are known as menisci. They function as the natural “shock absorbers” protecting the joint. The thigh and shinbones are held together by large ligaments, lending stability to the joint whereas the long thigh muscles make the knee strong. All remaining surfaces of the knee are covered by a thin lining called the synovial membrane. This membrane secretes a liquid that moistens the cartilage, minimizing friction to almost zero in the case of a healthy knee. Normally, all of these components work in harmony. But disease or injury can disrupt this harmony, resulting in pain, muscle weakness, and reduced function.
Although there are more than 100 types of Arthritis, the three most common types are Osteoarthritis, Rheumatoid arthritis and Post-traumatic arthritis. In this article, we will majorly focus on Osteoarthritis.
What is Osteoarthritis (OA)?
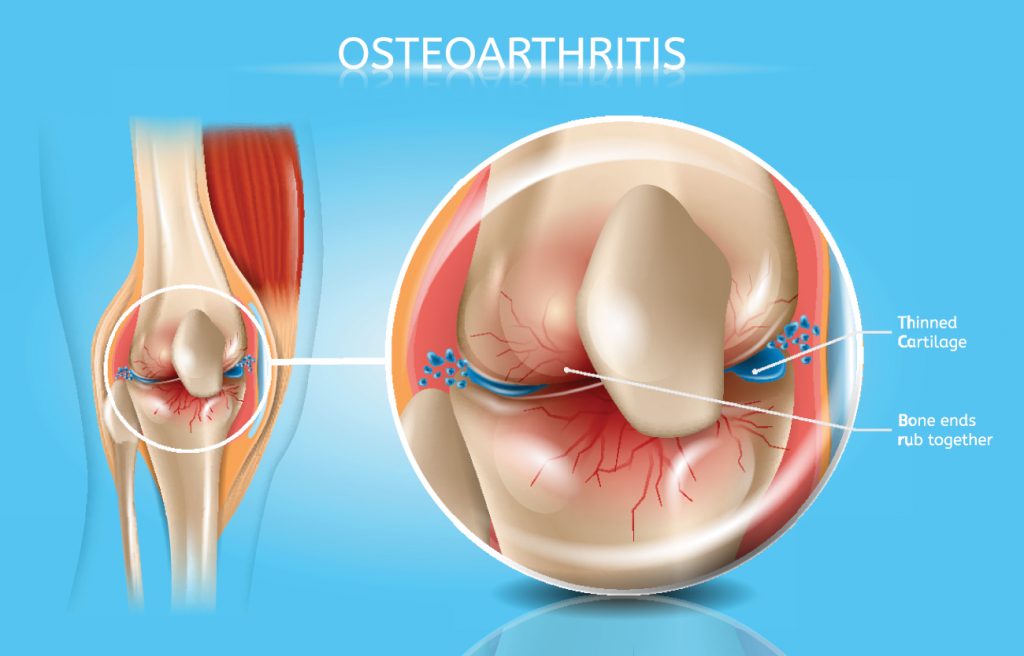
Osteoarthritis is an age-related “wear and tear” type of arthritis. It generally affects persons aged 50 years or more, but may also affect younger individuals. In this type of arthritis, the cartilage that cushions the bones of the knee softens and wears away. The bones then rub against one another, causing knee pain and stiffness. Osteoarthritis (OA) of the knee happens when the cartilage, the cushion between the knee joints deteriorates. This can cause pain, stiffness and swelling. Appropriate treatment can help relieve discomfort and slow the damage. It can also improve your quality of life facilitating you to better keep up with your day-to-day activities.
What are the causes of Osteoarthritis?
- Age: The risk of developing OA increases as someone gets older because bones, muscles and joints are also aging.
- Joint injury
- Using the same joints over and over in a job or sport can result in OA.
- Obesity: Extra weight puts more stress on joint and fats cells to promote inflammation.
- Weak muscles: Joints can get out of the right position when there’s not enough support.
- Hereditary: People with family members having OA can also suffer from OA.
- Women are more likely to develop OA than men.
What are the signs & symptoms of OA?
- Joint stiffness and soreness
- Grating sensation
- Bone spurs
- Loss of flexibility
- Pain or aching in the joint during activity
- Limited range of motion that may go away after movement
- Clicking or cracking sound when a joint bends
- Swelling around a joint.
How to Diagnose Osteoarthritis?
Osteoarthritis of the major joints is most effectively diagnosed through a combination of medical history, physical examination, and various lab tests including imaging studies such as X-ray. A physician can diagnose most of the cases but in some cases, he may refer you to an Orthopedic surgeon, physiatrist for further evaluation.
Medical History
Medical histories can often be the most useful tool for physicians in diagnosing osteoarthritis. The doctor will look for a family history of the disease as well as the presence of various risk factors to indicate the need for further testing.
Physical Examination
A physical examination will usually follow the medical history as the physician looks for physical signs of the disease. These include signs like swelling and tenderness of the joints, loss of movement in specific joints, or visible joint damage such as bony growths in the surrounding area. The patient may also be asked to perform a variety of physical tasks so the physician can evaluate the range of motion and general joint mobility.
What are the treatment options for Osteoarthritis?
General Management
Patients with osteoarthritis of the hand may benefit from assistive devices and instruction on techniques for joint protection; splinting (a rigid or flexible device that maintains in position a displaced or movable part) is beneficial for those with symptomatic osteoarthritis.
Patients with mild to moderate osteoarthritis of the knee or hip should participate in a regular exercise program (e.g. a supervised walking program, hydrotherapy (water cure) classes) and, if overweight, should follow a healthy and balanced diet. The use of assistive devices can improve functional status.



Medical Management
- Oral nonsteroidal anti-inflammatory drugs (NSAIDs) – Common NSAIDs are ibuprofen and diclofenac; painkillers.
- Topical therapies – Topical NSAIDs are applied to unbroken skin where it hurts in the form of gels, creams, sprays, or plasters.
- Intra-articular injections – A term used to define a shot delivered directly into a joint with the primary aim of relieving pain.
Surgical Measures
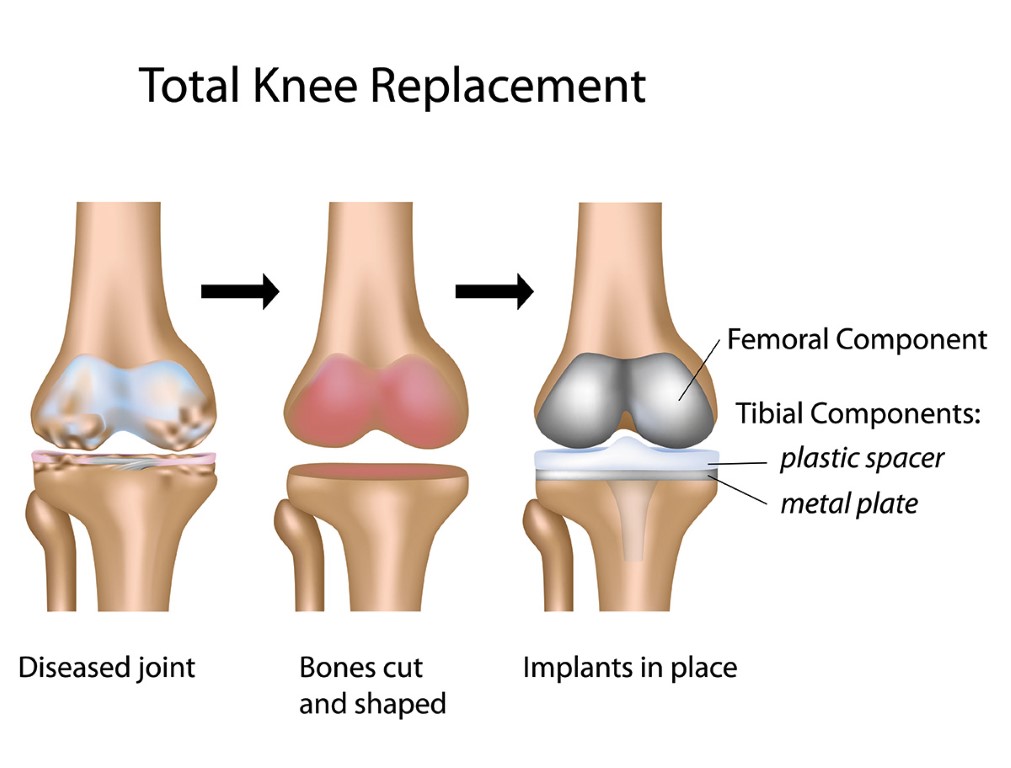
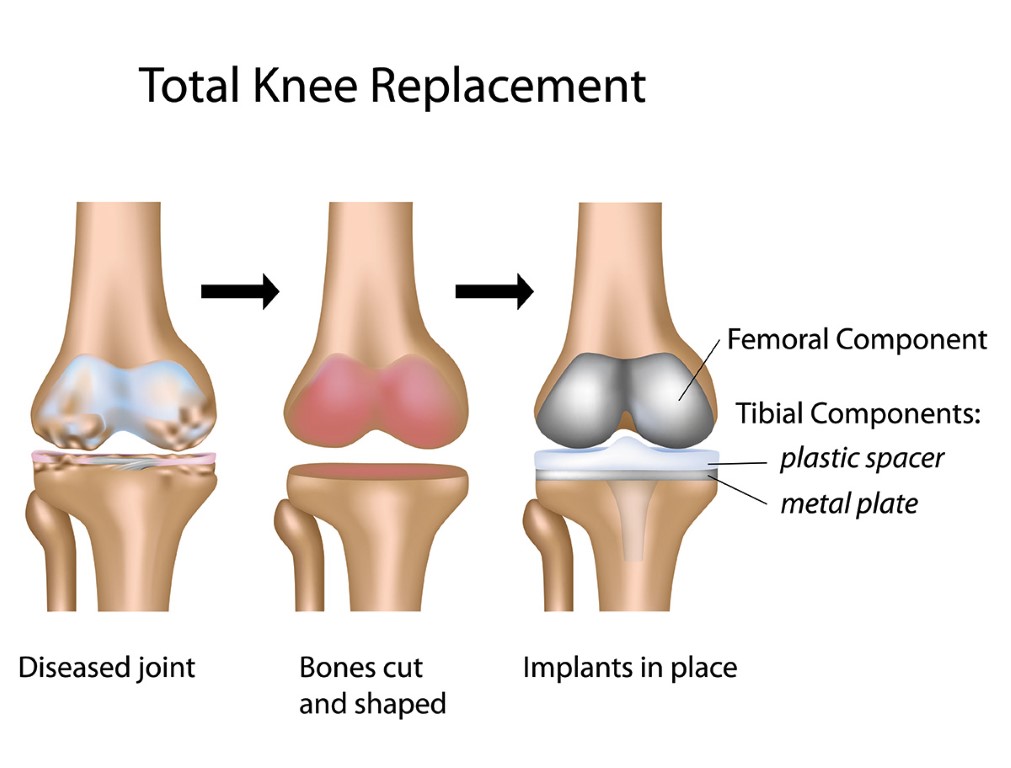
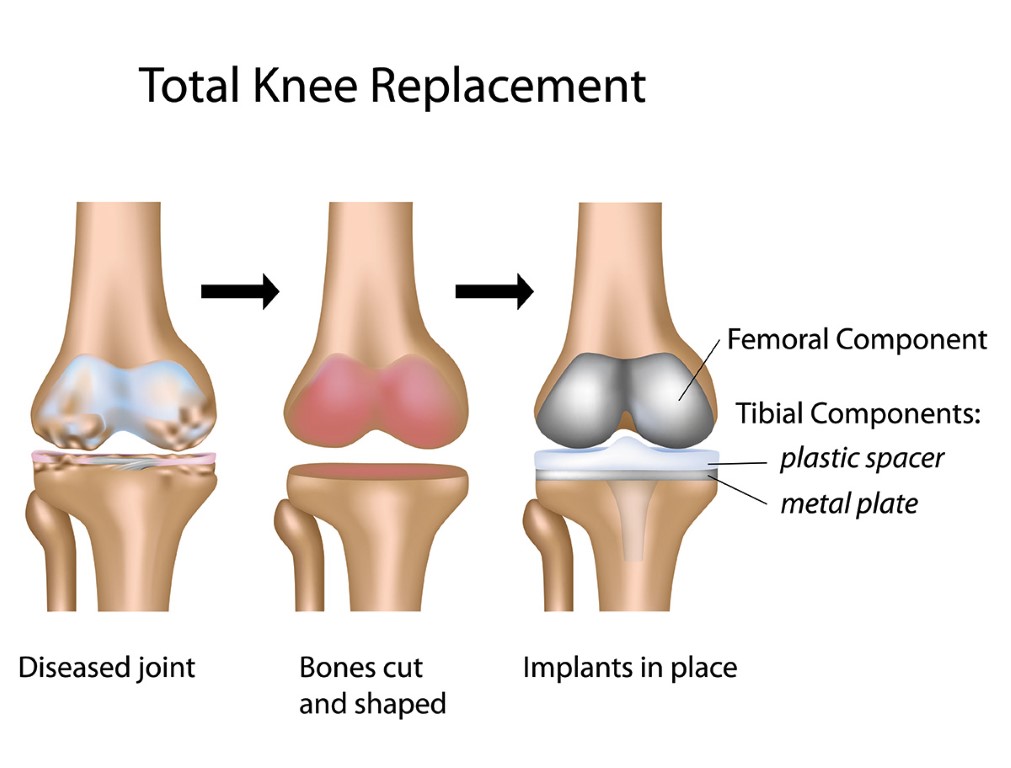
Total hip and knee replacements provide excellent symptomatic and functional improvement when the involvement of that joint severely restricts walking or causes pain at rest, particularly at night. Total Knee Replacement is one of the most common surgeries in the world with a large majority of patients going on to lead rich, happy and healthy lives. It requires a surgery of 1-2 hours followed by a hospital stay of 2-3 days.
The knee is the human body’s largest joint and is made up of the lower end of the thighbone, the upper end of the shinbone and the kneecap. A knee replacement includes replacing some or all of the component surfaces of the knee joint with artificial implants. A knee replacement is performed to repair the damaged weight-bearing surfaces of the knee joint caused due to inflammatory diseases or injury. The damage over time leads to extreme pain and can restrict joint mobility. Knee replacement is a major surgical procedure requiring hospital admission for 2 to 3 days.
Depending on the severity of the disease your doctor will suggest the best line of treatment to treat Osteoarthritis.




