Arthritis is an unwelcome guest that barges into the lives of countless individuals, bringing joint pain and inflammation. Today, we will compare and contrast the two common types of arthritis: Osteoarthritis and Rheumatoid Arthritis. While both share similarities in joint discomfort, they have distinct characteristics that set them apart. So, let us embark on a journey to unravel their causes, symptoms, risk factors, diagnosis, and available treatments.
Osteoarthritis
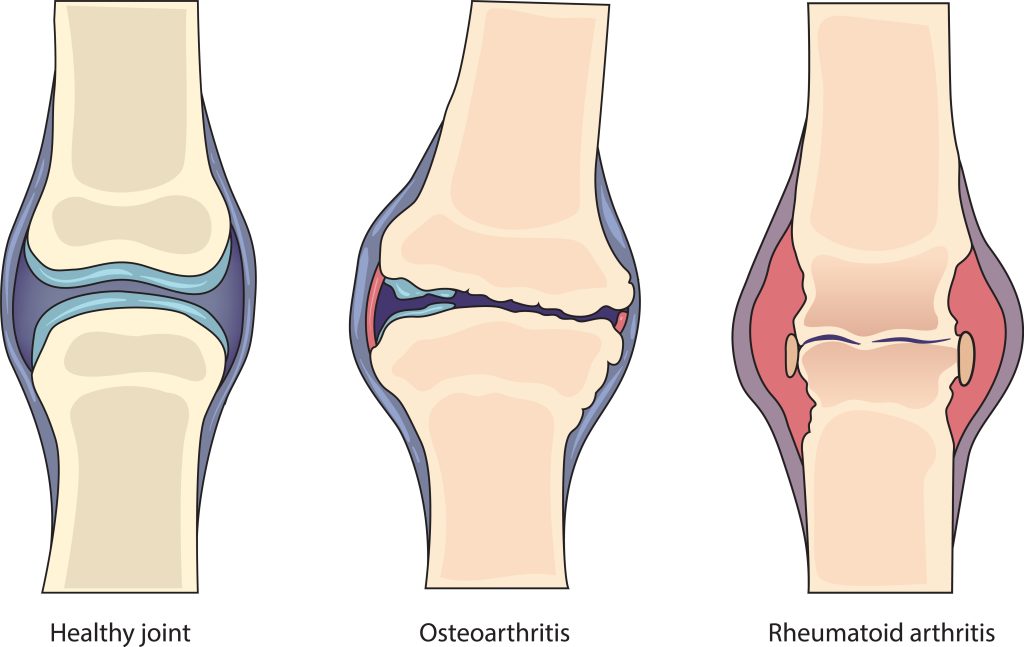
It typically occurs as a result of wear and tear on the joints. Cartilage, the tissue which covers the ends of bones within a joint, is mainly impacted by this condition. Over time, the cartilage breaks down, leading to pain, stiffness, and reduced joint mobility. In addition, factors like aging, obesity, joint injuries, and repetitive joint stress can contribute to OA development.
Osteoarthritis symptoms include joint pain, swelling, tenderness, stiffness, and a decreased range of motion. These symptoms often worsen after periods of inactivity or excessive joint use. Osteoarthritis most commonly affects joints, including the hips, knees, hands, and spine.
Diagnosing osteoarthritis involves a combination of a physical examination, medical history review, and imaging tests such as X-rays or magnetic resonance imaging (MRI). These tests help evaluate the condition of the joint and rule out other potential causes of the symptoms.
Rheumatoid Arthritis
It is an autoimmune disorder wherein the immune system mistakenly attacks the body’s healthy tissues. It primarily targets the synovium—the lining of the joints. This chronic inflammation leads to joint pain, swelling, and stiffness, and if left untreated, can result in joint deformity and functional impairment.
The cause of rheumatoid arthritis is still unidentified. However, experts believe that it involves a combination of genetic predisposition and environmental triggers. Women are more commonly affected by rheumatoid arthritis than men, and it often develops between 30 and 60.
The symptoms of rheumatoid arthritis include joint pain, swelling, morning stiffness lasting more than an hour, fatigue, and a general feeling of malaise. Rheumatoid arthritis can affect multiple joints simultaneously, including the wrists, hands, feet, and knees. In some cases, it may also involve other organs, such as the lungs or heart.
A thorough examination of symptoms, medical history, and blood tests such as rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies may be required to diagnose rheumatoid arthritis. In addition, imaging tests like X-rays and ultrasounds may also be used to assess joint damage and inflammation.
Differences Between Osteoarthritis and Rheumatoid Arthritis
Osteoarthritis and rheumatoid arthritis affect the joints, resulting in pain and stiffness. However, they differ significantly in their underlying causes and characteristics. Osteoarthritis is known to be primarily caused by wear and tear. Conversely, rheumatoid arthritis is an autoimmune condition.
Osteoarthritis generally develops later in life, often after 50 years of age, and is common in individuals with a history of joint injuries, obesity, or occupations involving repetitive joint movements. Rheumatoid arthritis, on the other hand, can occur at any age and tends to affect more women than men.
In terms of disease progression, osteoarthritis usually develops gradually over time. In contrast,
rheumatoid arthritis can have a more rapid and aggressive onset, with symptoms often affecting multiple joints simultaneously. In addition, without appropriate treatment, rheumatoid arthritis can lead to joint deformities and functional limitations, whereas osteoarthritis is typically less severe in its impact.
Osteoarthritis and rheumatoid arthritis have different treatments. For osteoarthritis, the focus is on pain management, lifestyle modifications, physical therapy, and possibly nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroid injections to reduce inflammation. In some severe cases, joint replacement surgery might be necessary.
In contrast, rheumatoid arthritis requires a more comprehensive approach. Treatment aims to reduce inflammation, manage pain, and slow disease progression. Medication is commonly prescribed to control inflammation and suppress the overactive immune response. Physical therapy, assistive devices, and joint protection techniques are essential for managing rheumatoid arthritis.
Conclusion
In conclusion, osteoarthritis and rheumatoid arthritis are distinct forms of arthritis with different causes, symptoms, risk factors, diagnosis methods, and treatment approaches. Osteoarthritis primarily results from joint wear and tear, while rheumatoid arthritis is an autoimmune condition. Understanding the differences between these conditions helps to accurately diagnose and appropriately manage the condition, as tailored treatment plans can significantly improve the quality of life for individuals with arthritis. If you experience joint pain or suspect you may have arthritis, consult a healthcare professional for an accurate diagnosis and personalized treatment approach.
FAQs
Q: What is the difference between osteoarthritis and rheumatoid arthritis?
A: Osteoarthritis is primarily caused by joint wear and tear, while in rheumatoid arthritis, the immune system mistakenly attacks the body’s healthy tissues.
Q: How do the symptoms of osteoarthritis and rheumatoid arthritis differ?
A: Osteoarthritis symptoms include joint pain, tenderness, stiffness, swelling, and reduced range of motion. Rheumatoid arthritis symptoms include joint pain, swelling, morning stiffness lasting over an hour, fatigue, and general malaise.
Q: What are the associated risk factors of osteoarthritis and rheumatoid arthritis?
A: Risk factors for osteoarthritis include aging, obesity, joint injuries, and repetitive stress on the joints.
Q: How are osteoarthritis and rheumatoid arthritis diagnosed?
A: Osteoarthritis is diagnosed through a physical examination, medical history review, and imaging tests such as X-rays or MRI. Rheumatoid arthritis diagnosis involves examining symptoms, medical history, and blood tests such as rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies.




Comments are closed.