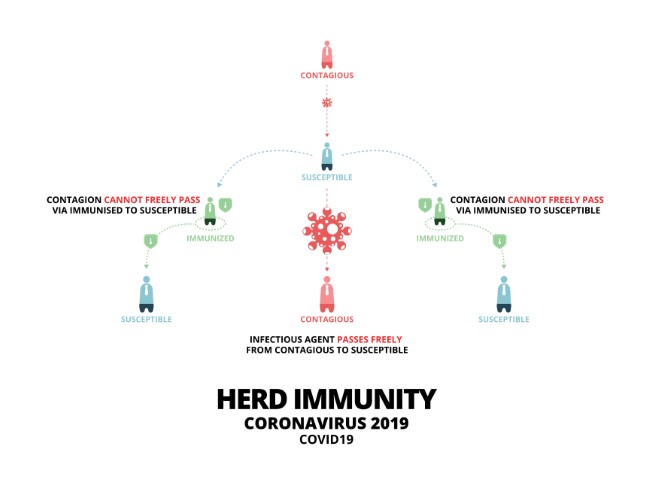
The COVID-19 pandemic has shaken the world and brought about drastic changes in our lives. As each wave is hitting stronger than the other, there is an increased demand for COVID tests and vaccines. With cases increasing day by day, there is a lot of pressure on labs and diagnostic centers to give out the test reports immediately, so that a person can start with the treatment and medications if tested positive. Also, to get tested, people would have to be physically present in the testing center, waiting in queues, exposing themselves to viruses, and increasing the risk for the people around them too. According to medical experts, the results must be given quickly, normally within 24 hours, to prevent the transmission of the virus. And delayed test results lead to further delay in treatment.
To avoid these problems and reduce the burden on the labs and diagnostic centers, the Indian Council of Medical Research (ICMR) given its approval for the COVID-19 Home Testing Kits. These Home Testing Kits are easily available in pharmacies and are one-stop solutions for all the problems with the traditional COVID tests.
What are self-test COVID-19 Rapid Antigen Kits?
These are Rapid Antigen Tests (RATs) that are available with the required device along with accessories to test oneself at home. These self-tests can be used to detect both symptomatic and immediate contacts of confirmed cases, as per ICMR guidelines. These over-the-counter self-testing kits do not require a prescription.
A positive test result should be considered as a true positive & does not need reconfirmation by the RT-PCR test.
Negative results must be combined with clinical observations, patient history, and epidemiological information. Symptomatic individuals identified negative by Rapid Antigen Test (RAT) should be linked with RT- PCR test facility and subsequently get tested by RT-PCR to rule out COVID-19 infection. In the meantime, such individuals will be urged to follow home isolation and treatment as a negative report on RAT may not be true negative in some cases.
Who can use the COVID-19 Home Testing Kits?
The test can be used on people who display symptoms of COVID-19 or are high-risk contacts of positive patients. The COVID-19 home test can be used on people who are 18 years of age and above, and even as young as children who are 2 years of age, when the samples are collected by an adult.
What are the contents available in the self-testing kits?
In each self-testing kit, there is an instruction for use leaflet, all the required testing materials, and a biohazard bag for disposal. The testing materials include a nasal swab, test card, and an extraction tube filled with an extraction solution along with Cap.
How to use the COVID-19 Rapid Antigen Self-test Kit?
Before testing yourself, pick a comfortable spot to take the test. After finalizing the place, wash your hands or sanitize them thoroughly. Also, ensure that the surface on which the kit will be placed is cleaned and disinfected. After opening the contents of the kit
- Remove the swab from the package. Do not touch the soft end with your hands or anything else.
- Insert the swab gently into your nostril about 2-4 cm or until resistance is met,
- Roll the swab 5 times inside the nostril
- Use the same swab and repeat this process in the other nostril
- Place the device on a clean, flat surface
- Peel off the aluminum foil from the top of the extraction solution tube
- Insert the nasal swab sample into the extraction solution, and then mix the swab 8 to 10 times
- Squeeze the swab by the side of the extraction tube and break the swab at the breakpoint, remove the remainder of the swab and mix well
- Place the dropper cap tightly onto the tube and add 4 drops (100uL) into the sample well
- Start the timer and wait for 15 mins for the results to show up.
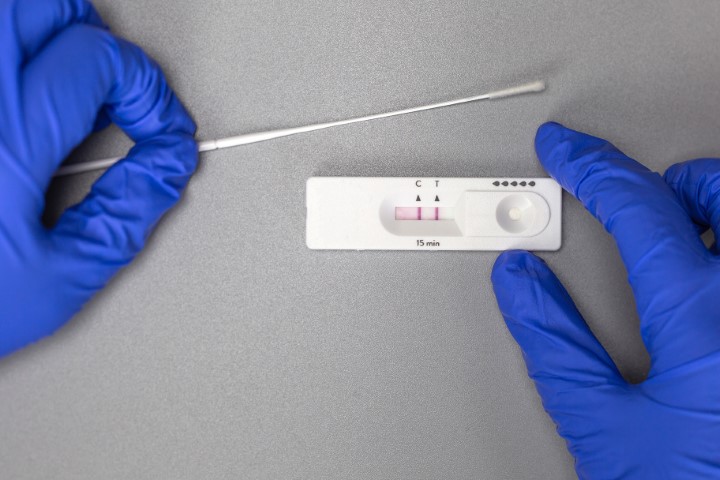
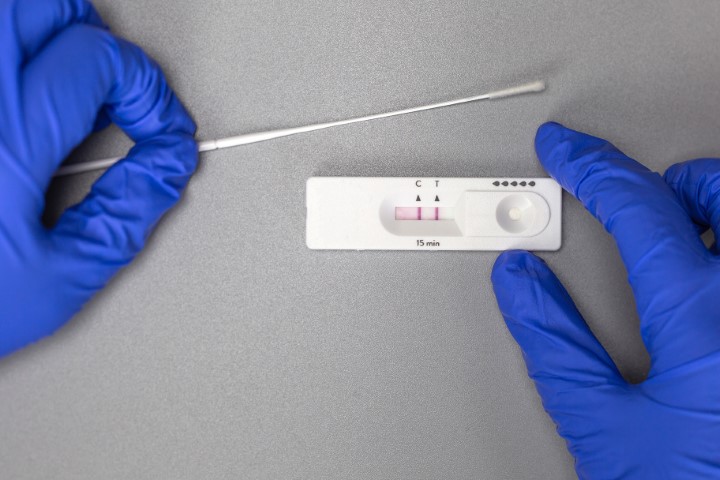
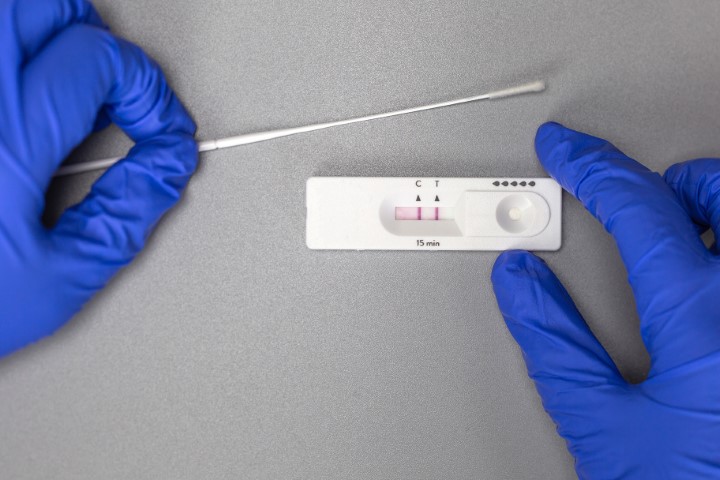
How will I know I have tested positive?
The test will take 15 – 20 minutes to show accurate results. If both the control band “C” and the test band “T” marked on the testing card are developed, the result is positive. If only the control band “C” is developed and the test band “T” is not developed, it means that the result is negative. If neither the control band nor the test band develops, or if only the test band develops without the control line, it means that the test is invalid.
How to dispose the COVID-19 Antigen Rapid Test Kit?
Whether the results are negative or positive, one must dispose of every item from the kit. After using the kit, put the test device, swab, and the extraction tube in a biohazard disposable bag and put it in the bin.
What are the disadvantages of the Home Testing Kit?
One of the biggest disadvantages of the self-testing kits is the reliability. Though these home tests yield quick results and minimize exposure to the virus, there are chances of the result being negative or invalid if the sample is not being collected correctly, or the swab getting contaminated, which also leads to inaccurate results. Hence, if the home test results are negative and the person still displays symptoms of COVID-19, one must follow up with their healthcare provider for further advice and stay in isolation till confirming test results are received.
These Rapid Antigen COVID-19 Home Testing Kits are helpful in the early detection of the condition. While self-testing, it is extremely important to follow the instructions of your healthcare provider carefully. Although it’s a game-changer during this time, it is important to understand that it is a screening test and to be used as an aid in the diagnosis of SARS-CoV-2 infection and cannot replace the confirmatory testing method. So, positive or not, always get in touch with a medical health expert and follow their advice for more information and quick recovery.