Introduction
The natural aging process changes the body, biologically, physiologically and psychologically, along with other changes increasing older people’s susceptibility to disabilities and diseases. The term Geriatric means “of old age” and often refers to older people’s health conditions such as osteoporosis and dementia and healthcare. There is an increased risk for fractures in older people due to the bones getting weaker and losing strength and density. That’s why it is essential to know the signs of a fracture in the elderly so you can take action before an injury becomes more serious. If you have an older family member or friend, they’ve likely experienced a broken bone or two. After all, an estimated 71% of adults will break a bone at some point. However, this doesn’t mean that everyone experiences fractures in the same way or at the same rate as others.
What are Geriatric Fractures?
Geriatric fractures are broken bones that affect older people more often than not. There are several different types of geriatric fractures, each associated with a health condition and resulting in different symptoms. Fractures more often than not happen due to falls, accidents, or as a result of a direct impact or trauma to the affected body part.
Types of Geriatric Fractures
The two most common geriatric fractures are osteoporosis-related fractures and falls-related fractures. Osteoporosis-related fractures occur when older adults with osteoporosis have low bone mass, bone strength, and low bone density. This makes their bones more likely to fracture. Falls-related fractures occur when an older adult has low bone density and falls because they are not as strong as they used to be. This can happen because their balance is affected by a related medical condition such as dementia or the side effects of medication. Other types of geriatric fractures include fractures associated with poor muscle function and bone infections.
Symptoms of Geriatric Fracture
The most common symptom of a bone fracture in the elderly is pain and impairment of mobility. However, if the fracture is causing other symptoms, it’s necessary to see a doctor.
- Pain in the limb that is difficult to explain, for example, or pain that goes away when the limb is bent, can be a sign of a fractured bone.
- Limping or having a hard time walking can be a sign of a more serious injury and should not be ignored.
- Redness, swelling or warmth, or bruising around the broken bone can indicate a more serious injury and should be a concern.
- Loss of strength in the arm or leg can indicate a more serious injury.
- A feeling of obvious deformity or change in how the broken bone feels can indicate that the bone has shifted or moved inside the joint, which can signify a more serious injury.
Risk Factors for Geriatric Fractures
Geriatric fractures like hip fractures can be debilitating with increased mortality, loss of independence, and long-term disability. Hence, we must pay enough attention to the risk factors for Geriatric Fractures and work towards fracture prevention and patient education.
Poor bone health: People with osteoporosis and low bone mass are at an increased risk for
fractures. Osteoporosis is a condition that occurs when bones lose too much bone density.
The bones become weak and more fragile, leading to associated disorders like low body weight, malabsorption syndromes like chronic liver disease (CLD) and inflammatory bowel disease, primary hyperparathyroidism, rheumatoid arthritis, and long-term immobility.
- Dementia: People with dementia lose the cognitive functioning of the brain. They become forgetful, and their thinking gets impaired, affecting their daily life. These people are more prone to accidents and falls and are also likely to have low bone density, thereby increasing the risk of fractures.
- Medication side effects: People who take medication to control blood pressure, reduce glucose levels, or control seizures are at an increased risk of fractures due to changes in their balance and strength.
- Obesity: Obese are at an increased risk of osteoporosis and fractures. Obesity affects more than just your looks and is also associated with an increased risk of fractures.
- Poor Lifestyle and Behavioral Factors: Sedentary lifestyle, poor eating, sleeping, lack of physical activity, and unregulated drinking and smoking contribute to poor bone health and associated complications. Those with low calcium intake, vitamin D deficiency and lack of physical activity are equally at risk.
How are Geriatric Fractures Diagnosed?
It is often difficult to diagnose a geriatric fracture with/without any health conditions causing them. The doctor will ask about signs and symptoms, complete medical history of both patient and general family health to determine if there are underlying health conditions or any other risk factors for fractures associated with advancing age, and physically examine and try to determine the type of fracture by ordering for the following tests to help make the diagnosis,
- an X-ray
- a magnetic resonance imaging (MRI) scan
- or a Computed tomography (CT) scan
Prevention of Geriatric Fractures
It is beyond our control to prevent or predict geriatric fractures caused by falls, accidents, and other injuries. As a silent epidemic, increasing fractures among the elderly are becoming a major public health concern. It is a priority to prevent fractures in older people or people over 65. The challenge is to identify those at most risk, especially those who have previously had a fall, intervene and assess risk levels, and ensure timely and cost-effective treatment. Awareness about improving bone health and reducing any risk of injury is a must.
- A calcium and Vitamin D-rich diet to keep bones healthy and strong.
- Follow a weight-bearing exercise regime to keep bones strong.
- Complete abstinence from smoking. Tobacco and nicotine increase bone fracture risk and slow down the healing process.
Treatment of Geriatric Fractures
As an older person, if you’re concerned about your symptoms or have a broken bone that doesn’t cause other symptoms, don’t wait to see a doctor. Do not attempt to treat the fracture yourself. The most important thing to do is protect the injured limb, put the broken pieces of the bone back in place, expedite medical intervention to heal to reduce the pain and trauma, and avoid any complications.
Treatments typically include –
- putting the fractured bone in a splint or cast
- medication to reduce/control the pain
- traction to stretch the muscles and tendons around the injured bone to help alignment and healing, and
- surgery to fix certain types of fractured bones into place. Surgery involves the installation of metal rods or pins inside the bone or outside the body to hold the bone fragments in place for them to heal.
The prognosis for Geriatric Fractures
The prognosis for a geriatric fracture is good if the fracture is diagnosed early and treated properly. But if it is not managed properly, it can result in serious complications. It’s crucial to protect an injured limb and see a doctor. In many cases, the fracture can be treated with medication, surgery, or a combination of these procedures. It’s important to know that even when the fracture heals, some changes in the bone may be permanent.
Conclusion
Fractures are a serious risk for older adults, especially those with low bone density, a fall-related or osteoporosis-related fracture, or a fracture associated with poor muscle function. For these reasons, it’s important to know the signs of a fracture and protect yourself from injury. If you notice any sign of a fracture, don’t hesitate to see a doctor. They can help protect your health and avoid serious long-term damage.
FAQs
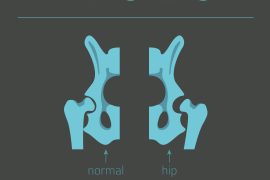
What type of fractures is most common in the elderly?
Older people are at high risk of bone fragility, falls, and fractures. The most common fractures among the elderly are hip fractures, accounting for at least 90 percent. Typically, all appendicular fractures are precipitated by a fall.
Why are fractures common in the elderly?
Fractures are most common in the elderly because of advancing age, bones getting weaker and brittle due to osteoporosis, and an unfortunate fall. The bones get more fragile with age with the natural bone tissue changes. For women, especially after menopause, the bones get weaker and thinner with the decline in the female hormone estrogen.
Why do the elderly take longer to heal fractures?
The elderly usually take longer to heal fractures because of the declining count of stem cells in the bone marrow due to old age. Recovery from a bone fracture requires sufficient vascularization and the formation of blood vessels in the tissue. Advancing age tends to hinder this process by preventing crucial bone healing sites.
Can the elderly recover from fractures?
When the elderly experience a fall and a fracture, many recover fully, get back on their feet, and lead normal lives. The key lies in prompt action and dealing with all kinds of falls and fractures with precision and timely medical intervention in the case of any type of fracture involving the upper leg, knees, pelvis, hip, skull, back and neck.
How do you know if a fracture is healing?
Never mind how big or small a fracture is, there are 4 tell-tale signs to tell if a fracture is healing or not.
- Decreasing Pain – When the intensity of pain a fracture afflicted person experiences is on the decline.
- Improved Mobility – The healing period of a fracture can render a fracture-afflicted elderly patient pretty immobile. As the healing takes over, the mobility of the affected limb will improve.
- Lack of Bruising – When the area around a fractured bone shows no signs of bruising, the fracture is healing well.
- Decreasing Swelling – When the area around a fractured bone displays less swelling, know that it’s healing well.
Can an old fracture cause problems years later?
An untreated bone fracture can result in either a nonunion or a delayed union. When the bone doesn’t heal at all, it is called nonunion fracture. As a result, swelling, tenderness, and pain will continue to worsen. Delayed union fracture is when the bone takes more than the usual time to heal.
Can broken bones cause dementia?
The quality of life after an older person suffers from a fracture significantly affects the onset of
dementia. The after-effects of a bone fracture can result in less mobility and decline in physical agility, chronic pain, and prolonged inflammatory cytokine secretion during fracture repair can end up contributing to dementia.
When does a fracture stop hurting?
After a broken bone fracture of an older person is fixed by the doctor without surgery, the pain may subside significantly right after. However, an elderly person may experience some pain for up to 3-4 weeks and mild pain for up to 6-7 weeks after surgery.
What happens if a fracture doesn’t heal?
After a bone fracture, the body gets into a healing mode. If the broken parts of the bones are not properly aligned, the bone will go on to heal with a deformity called a malunion. This happens when a new bone occupies the huge space between the displaced ends of the broken bone.
What slows down bone healing?
High glucose levels and habits like smoking and drinking delay bone healing. For all elderly patients with fractured bones, being immobile for some time is a crucial factor in the treatment process. The healing process significantly slows down with any movement of bone fragments.




Comments are closed.