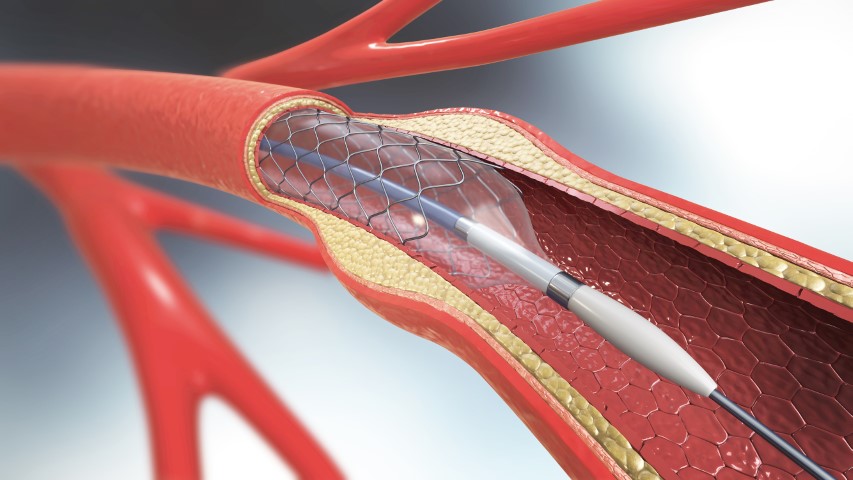
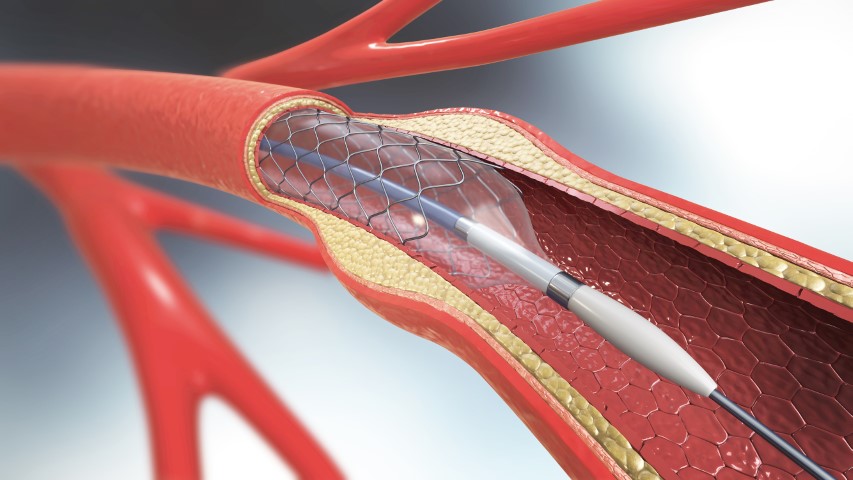
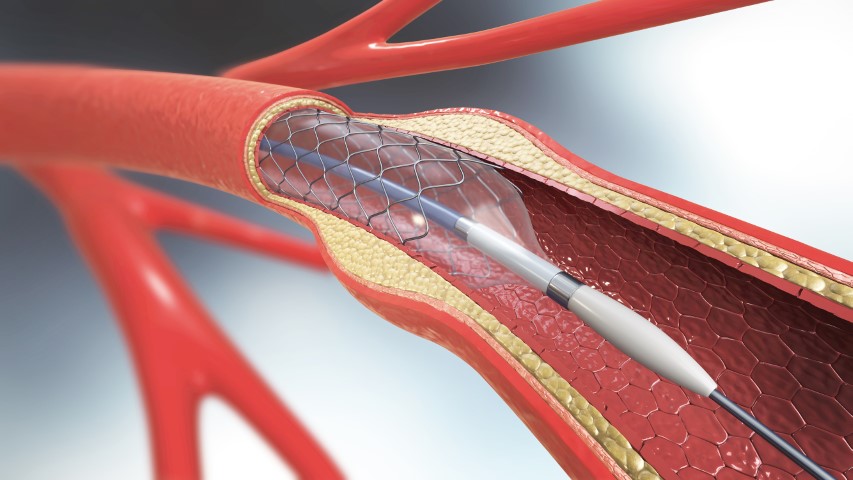
Heart disease often involves a problem with the valve, coronary arteries, or muscles all of which causes the heart to not function normally. The common heart disease among patients is CAD which arises from a build-up of plaque on the inner surface of the arteries. In the worst cases, it blocks the artery. Stents are instered to open the blocked artery and restor the blood by increasing the lumen area of the artery which got compromised due to plaque formation,it becomes even more important in the emergency like situation when patients suffer from the Heart Attack as due to thrombus a blood flow is totally stopped or compromised leading to the death of cardiac muscles due to lack of oxygen this need a immediate action to remove the thrombus or clot with help of medicines or angioplasty.
The idea of cardiovascular stents revolutionized the treatment of coronary-related diseases. Since then, stents have been used in coronary and peripheral procedures for decades. Let’s take a look at newer kinds of stents, their evolution and understand why better stents are needed.
What is the function of stents?
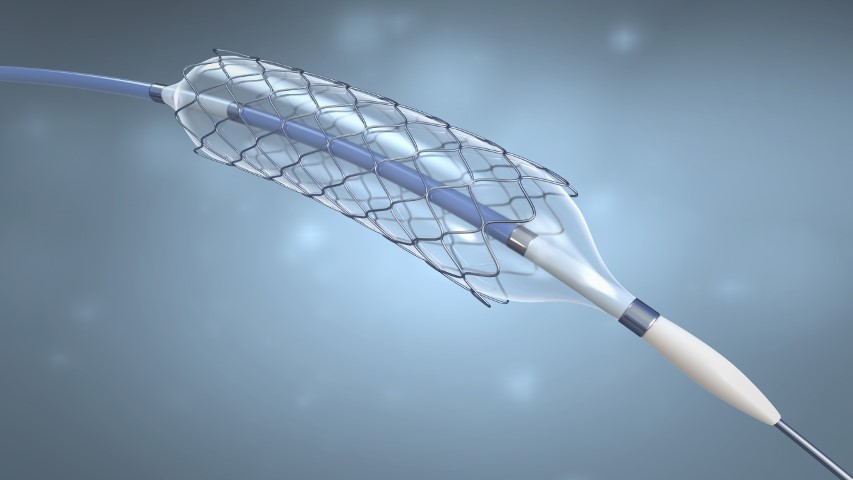
The main purpose is to open the blocked coronary arteries which occurred due to plaque formation. A stent is a tiny mesh tube inserted into a blocked passageway to keep it open, it restores the flow of blood. It is usually needed when plaque blocks blood vessels. Commonly used heart stents are made up of materials like stainless steel,cobalt chromium or platinium. It can be coated with medication to facilitae optimal healing.
Evolution of early stents
The first used stents were successful at reducing the risk of restenosis following angioplasty by about half, from 20% to 10% in the 12 months following the procedure. The first generation of stents was called bare-metal stents (BMS) as they were mostly fabricated from metal. These permanent frameworks are made from chrome steel and cobalt-chromium alloys for balloon-expandable and Nickel-titanium for self-expanding stents. This revolution was considered the turning point in the field of angioplasty however it had its disadvantages of increased risk of restenosis.
Stent developers started to coat bare-metal stents with polymers containing drugs that were aimed at inhabiting extra tissue growth at the site of the stent to reduce the rate of restenosis. These stents are called drug-eluting stents (DES). DES has been constantly developed by using several drugs.
DES has bought its advantage to overcome the limitation of BMS. Despite the influence in the clinical practice in vascular intervention, the major subject of the debate was incomplete endothelialization and hypersensitivity reactions to the polymer coating. The first-generation DES had all these drawbacks which had them failed. Due there coating material not being biodegradable or biocompatible their long-term efficiency was questioned. The potential risk associated with DES were late thrombosis and delayed healing.
The formation of a grume within the artery at the location of the stent is stent thrombosis. It is different from restenosis. Restenosis is the regrowth of tissue, it is a problem but it grows gradually so when it occurs there is time to treat it. In contrast, stent thrombosis tends to occur suddenly without warning, it commonly leads to the complete occlusion of the artery that then tends to produce a myocardial infarction (Heart attack) or sudden death.
In the youth of stenting, the matter of early thrombosis was recognized and successfully addressed by administering powerful antiplatelet or blood thiner for a couple of months after stenting. But within few years of the widespread use of DES the problem of late thrombosis was discovered. Late thrombosis may be a sudden thrombosis within the site of the stent that happens a year or two after the procedure. It is as catastrophic as early stent thrombosis. Hence the cardiologists started prescribing antiplatelet therapy for up to a year or for longer period of time. The strong use of anti-platelet drugs carried the risk. The problem of late stent thrombosis led stent developers to a challenge to develop a new type of stent that reduces this problem or eliminates it.
Researchers now believe that the polymer coating on DES may themselves increase inflammation and delay healing. Now several companies are identifying the problem and trying a general approach keeping this in mind.
Advanced stent technology
Better durable polymers DES appear to cause less inflammation and also allow better healing at the site of treatment. These stents are referred to as second-generation DES, the newer stent design use cobalt-chromium which has greater radial strength per thickness and is radio-opaque, and thus allows thinner struts.
Bioabsorbable polymers
DES has been available for several years, they employ a polymer coating which is absorbed within few months leaving just the bare stent. These stents offer the benefits of DES for several months then they become BMS. This reduces the risk of late thrombosis. As compared to the first generation DES the risk of late thrombosis is reduced with both second-generation DES and bioabsorbable polymers DES. But there is no indication that bioabsorbable polymer performs better than the second-generation DES. They both still require very prolonged therapy and anti-platelet tests.
Bioresorbable stents
Bioresorbable stents also called as bioresorbable scaffold, biodegradable stent, or naturally- dissolving stent they are made from a material that may dissolve or be absorbed in the body. The main purpose of the bioresorbable stents is to overcome the drawbacks of DES and BMS. Currently, A metallic drug-eluting stent remains in the body as a permanent implant which can lead to an increased risk of complications year on year. It may pose a hindrance if the future procedure needs to be performed in the same artery. But on the other hand, BRS provides a temporary scaffold to the lesion to restore the blood flow, once the blockage is treated and healed completely BRS dissolves on its own leaving the artery in its natural state with no foreign residue. Hence providing both physicians and patients the room to explore further treatment, if required in the same blood vessel.
We get to see all these extraordinary engineering in stent technology, it seems like sooner or later we might develop stents that would be able to eliminate the risk of both restenosis and thrombosis. But you need to make sure that before you agree to a stent talk to your doctor and explore options whether it will be helpful for you.




Comments are closed.