Introduction
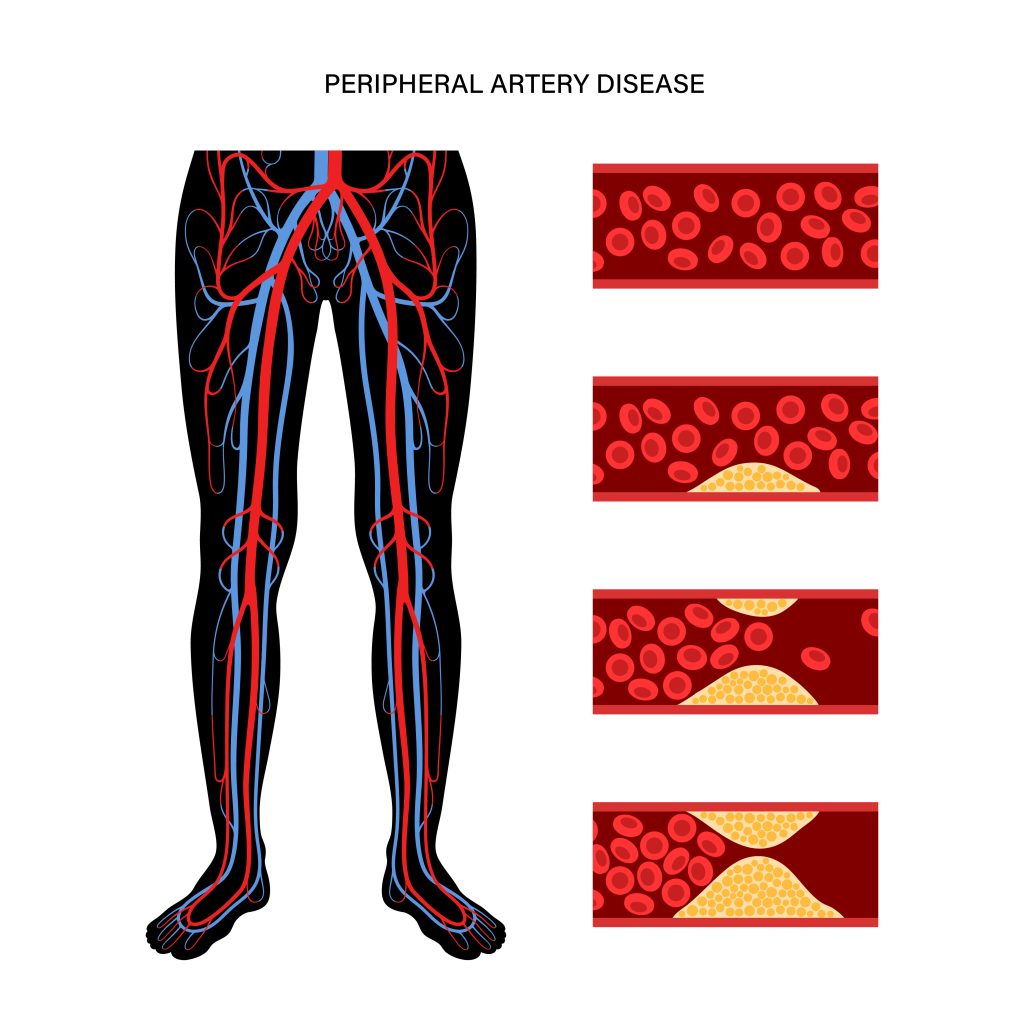
Arterial blockages are a slow and gradual narrowing of the blood vessels that carry oxygenated blood throughout the body. These blood vessels could be coronary (supplying blood to the heart), carotid (supplying blood to the brain and the head), peripheral (supplying blood to the body other than heart and brain), or renal (supplying blood to the kidneys) arteries that get blocked due to the accumulation of plaque (fibrous and fatty deposit) over time. This condition of plaque buildup, known as atherosclerosis, is the underlying condition in most arterial blockages. Also known as stenosis, blocked arteries hamper the regular smooth flow of oxygenated blood in the body, causing angina, claudication, kidney failure, high blood pressure, stroke, and other complications depending on the arteries affected by atherosclerosis.
Peripheral arterial disease (PAD) is one of the most common diseases with approx. two hundred million adults reportedly suffer from it, and the incidence increases to nearly 20% in older adults above 70 years. The disease affects the arteries of the extremities, often resulting in restricted mobility of the legs and the arms. The management and treatment for PAD starts with lifestyle changes, cardiovascular risk management, medications, alternate treatment modalities, or surgical or endoscopic treatment.
Continue reading this blog to know what to expect after peripheral artery stent replacement.
Peripheral Arterial Disease (PAD)
Atherosclerosis is the most common cause of PAD; the other causes may also include injury, inflammation, or exposure of the blood vessels to radiation therapy. The arteries of the legs and arms experience poor blood supply, causing symptoms of claudication (pain in the legs while walking and relief when at rest), and in extreme and severe cases, lead to gangrene.
People with diabetes, family history of PAD, smoking habits, obesity, high blood pressure, and high cholesterol are highly prone to developing the symptoms of PAD.
Lifestyle changes through a healthy diet, regular exercise, quitting smoking, stress management, and staying active helps control diabetes, blood pressure, cholesterol, and obesity, the contributing risk factors to PAD.
The treatment therapies aim to reduce the risk of PAD and improve mobility through exercises and walking. Patients less responsive to other therapies and lifestyle changes may need endovascular intervention
The procedure with a minimally invasive approach opens the blocked arteries by pushing the plaque to the arterial walls and placing the stent in the treated arteries. The procedure allows the smooth supply of blood to the extremities. Stents have been used for treating arterial blockages with high success and acceptance rates. Stents do not cure atherosclerosis. They treat the condition and relieve the patient from pain, discomfort, immobility, and dependence. Post-procedural care and management of the disease is a must for healthy living. Endovascular treatment with stent placement relieves the patient from the pain, inflammation, and discomfort associated with blocked peripheral arteries.
Alternatively, patients suffering from PAD can undergo a surgical treatment where a vascular surgeon cuts open the affected area and performs the procedure to cure the patient.
Life after Stent Placement
Stents are a boon for people who are misfit for surgery and/or non-responsive to other treatment options. The stent placement as a percutaneous procedure offers lesser pain, faster healing, fewer tissue scars, faster recovery, shorter hospital stay, and sooner resumption to routine.
The life of the patients undergoing stent placement for peripheral arterial blockages changes post-treatment. They experience significant relief from the symptoms of PAD. They can live a life of their choice once they have completely recovered. Life becomes relatively active and enriching, with people able to manage their daily chores comfortably and without stress and pain. They regain a sense of worthiness and purpose as they are less dependent on others for their daily needs.
However, the comfort and ease of living a life require post-operative care and management. One must pay attention to the fact that prevention is the only cure. The life of an individual after stent placement may seem like below.
- Immediately upon discharge from the hospital, the patient requires proper rest and downtime with physical activities for complete healing.
- Wound care (Diabetic patients) becomes a priority in order to prevent infection and other complications.
- Healing and recovery are faster with stent placement; compared to surgery, hence one is expected to resume routine in a week or two.
- One must adhere to positive lifestyle changes to prevent its relapse.
- With improved blood flow in the extremities, the patient feels less pain and more comfort in walking and staying active.
- The need for regular follow-up with the doctor and routine medications may arise is mandatory to keep a check on the condition.
Conclusion
PAD is a progressive condition, often a sign of poor cardiovascular health. The symptoms may or may not be noticeable earlier. For the treatment for PAD to be successful and effective, one has to take ownership for one’s health by being consistent in living a healthy life through positive lifestyle choices.
Life resumes normalcy faster after stent placement than open surgery. The relief from pain and discomfort makes life enjoyable and fulfilling. The benefits of stent placement for PAD are multiple, provided one takes precautions with wound care (diabetic patients), regular follow-up visits with doctors, a healthy diet, regular exercises, excessive physical stress to the legs and the arms, controlling risk factors, and a positive mindset.
References
Peripheral Arterial Disease – StatPearls – NCBI Bookshelf (nih.gov)


Comments are closed.