Introduction
Experience of any sharp pain or numbness in your legs after an extended period of sitting, painful cramps or aching in your hips, thighs, or calf muscles common and frequent after any physical activity, or coldness in lower feet, are signs of blockages in the arteries of the lower extremities. The condition is known as peripheral artery disease. As per reports, it is common, with nearly 41 to 54 million[1] estimated cases in India and nearly 4.2.to 6.2 million[1] people are afflicted by critical limb ischemia. According to the American Heart Association statement, approx. two hundred million people suffer from arterial blockages of the extremities worldwide.
The alarming statistics and the rising cases of other complications associated with arterial blockages in diabetic patients and people with smoking and alcohol consumption and/or obesity raise more significant concern for its stringent preventive measures and prompt and effective address.
The blog discusses the condition of arterial blockages, its causes, symptoms, and the treatment options for its effective control and management.
Peripheral Artery Disease- Its Causes and Symptoms
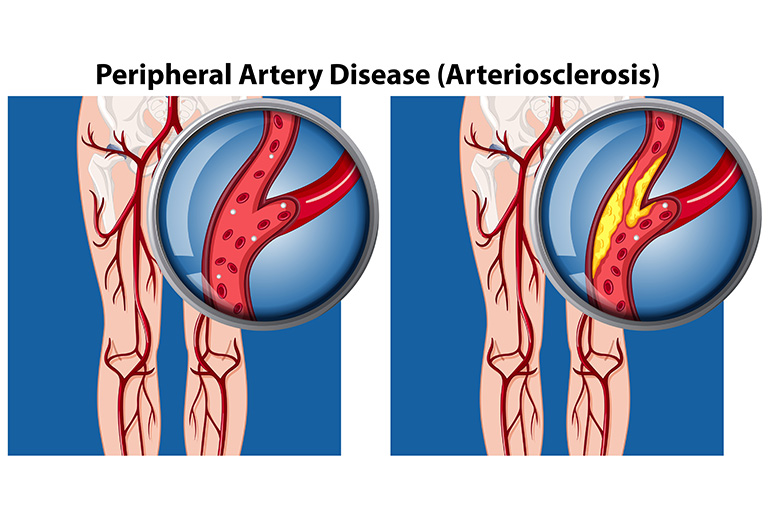
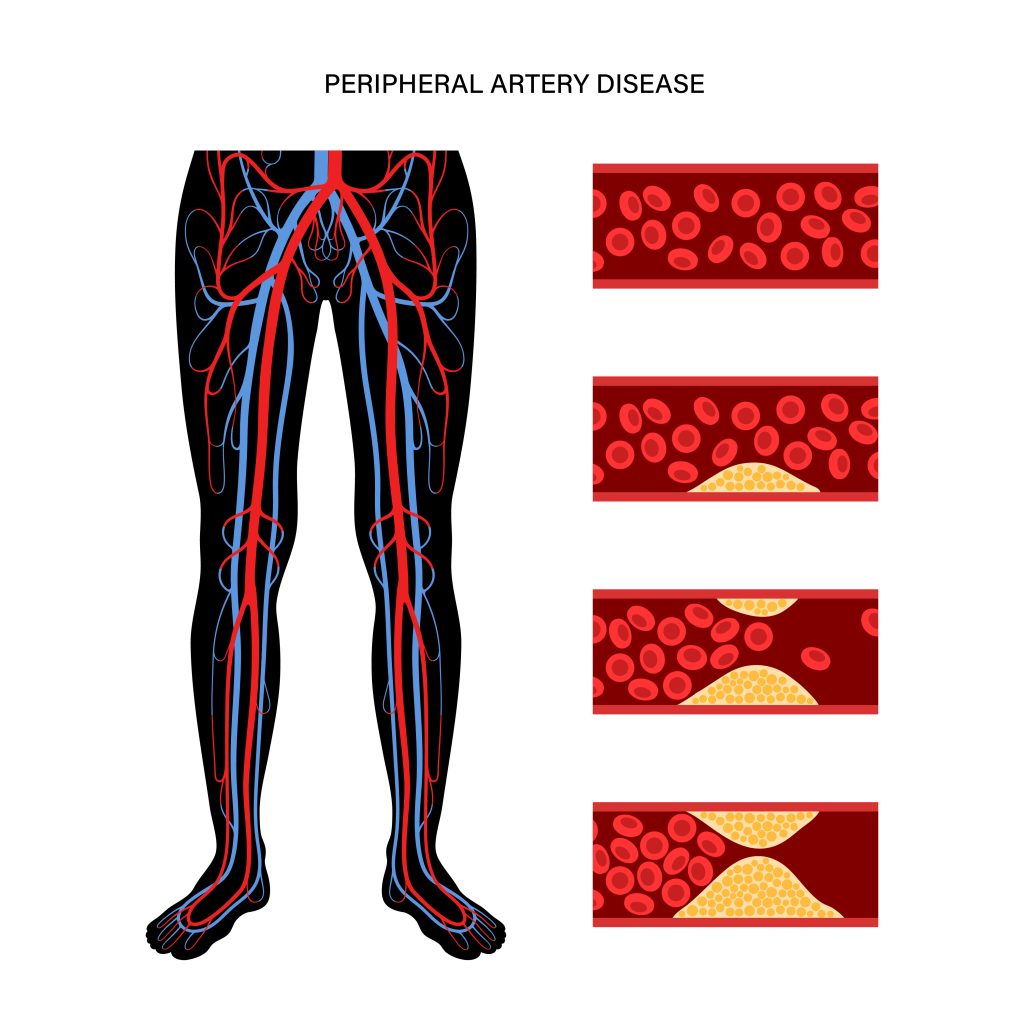
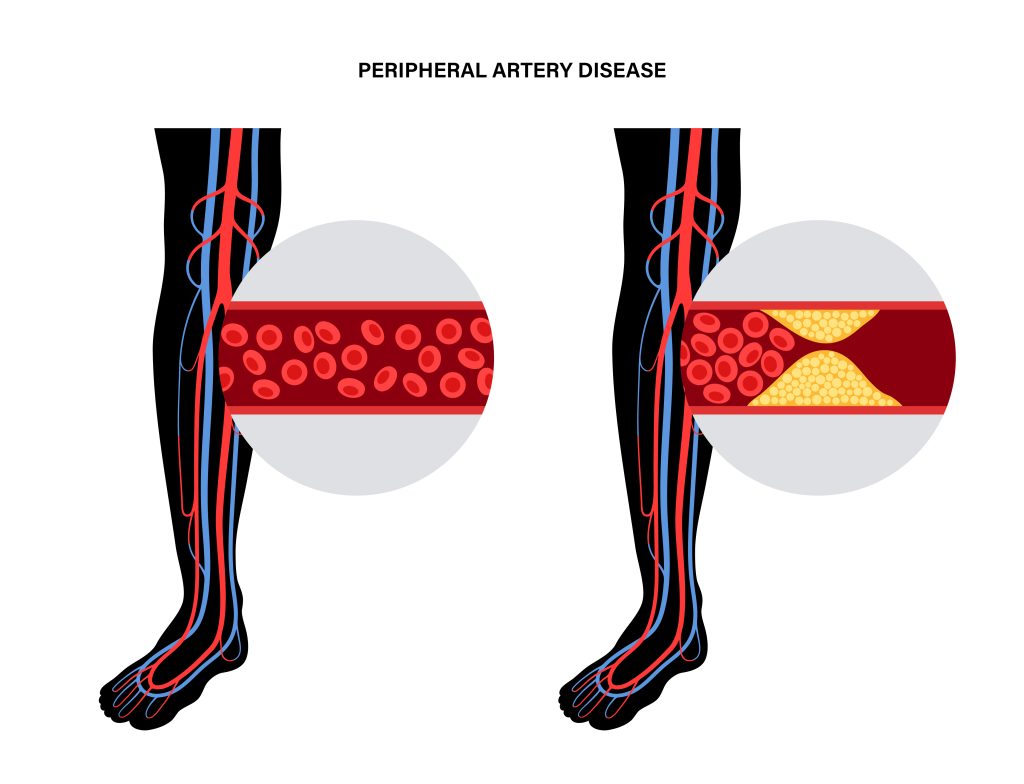
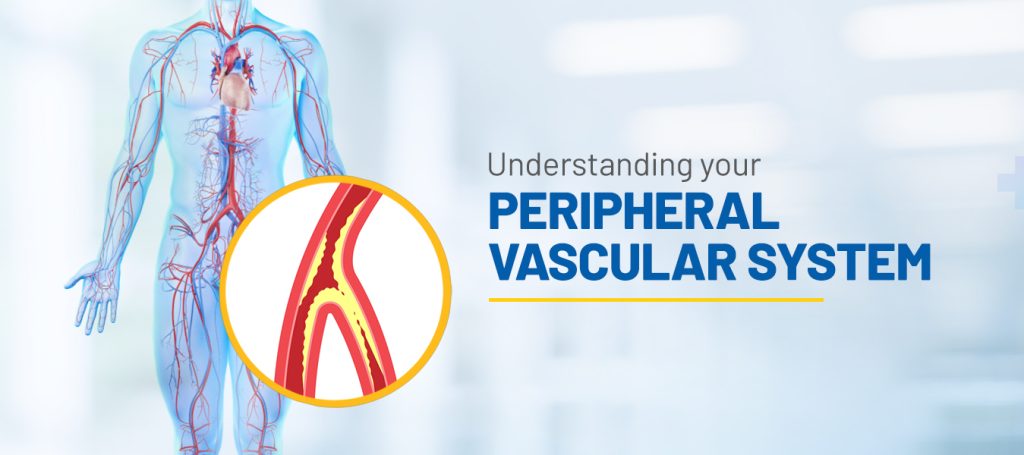
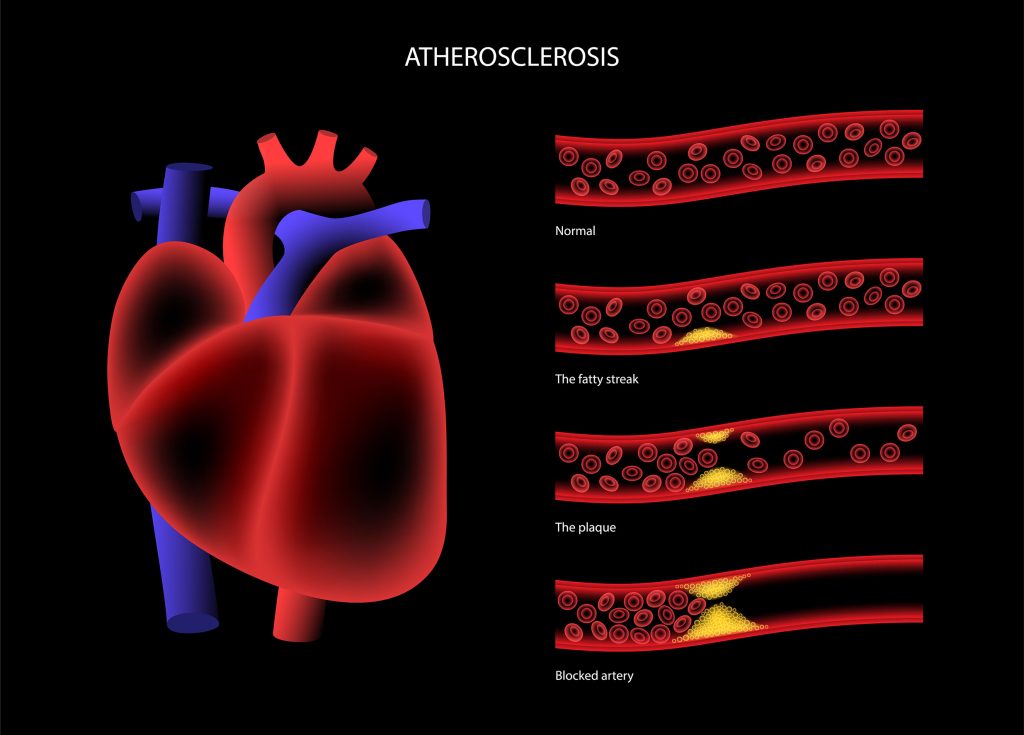
Peripheral Artery Disease (PAD) results from the narrowing of the arteries that carry blood from the heart to the peripheral arteries as well extremities, commonly the legs. The lack of oxygenated blood supply due to the narrowing of the arteries causes ischemic pain. The causes of arterial blockages are-
- Atherosclerosis – Plaque (fatty deposits) buildup over time results in the narrowing of the arteries, interrupting the blood supply to the peripheral arteries.
- Thrombosis– A clotting of the blood in the narrowed artery is one of the reasons for arterial blockages.
- Embolism– A condition of blocked artery caused by a blood clot or an air bubble in which the smooth flow of blood to the artery is interrupted, leading to an insufficient supply of oxygen. This causes pain, cramps, and other related symptoms of PAD.
Symptoms of PAD
People with PAD may not experience any symptoms until they become severe, which could at times adversely affect the heart health of the patient, if left unaddressed. This is so because PAD shares many common risk factors like diabetes, high cholesterol, high blood pressure, obesity, and smoking with heart disease.
The main symptom of PAD is claudication, where the person experiences flared cramping and pain in the legs and thighs when walking and subsides when at rest. The other symptoms include coldness in feet, numbness, tingling, or slow healing or unhealing of wounds.
Treatment for PAD
Preventing diseases and related complications is the best way to live a healthy life and enrich your quality of life. People with PAD are at a high risk of cardiovascular diseases and chances of stroke, heart attack, and other heart-related issues. Treatment for PAD requires rigorous and stringent healthcare precautions and aggressive lifestyle modifications.
Self-care and medications
A healthy diet, regular exercise, quitting smoking, management and control of comorbidities through medications, effective stress management, regular checkups, and monitoring through routine tests go a long way in preventing PAD and other related complications.
Surgical and non-surgical approaches
After the color doppler test, ankle-brachial index and vascular ultrasound test, the healthcare provider decides whether the patient needs surgical intervention to treat PAD. The severity of the condition is the primary and deciding factor for surgical intervention with other anatomical and health conditions of the patient.
Vascular Surgery
Known as open surgery or bypass surgery, the surgeon creates a new path around the blocked artery, using the healthy blood vessels from the other part of the patient’s body. This is known as grafting. The blood flows through the new path, bypassing the blocked artery.
During this bypass surgery, the patient is put on general anesthesia to keep them comfortable. The surgeon makes incisions to access the arteries and veins. The surgeon may use healthy veins like the saphenous veins (superficial veins in the legs), cephalic veins (veins from the arm), femoral veins (from thighs in case of more extensive artery grafting) from the patient’s body or use a synthetic material for grafting when natural healthy veins cannot be used. The surgeon sews the bypass in place and closes the incisions.
Endovascular Interventions
Atherectomy- It is a minimally invasive procedure to remove plaque from blocked arteries. During the procedure, the healthcare provider uses a sharp blade or laser attached to the tip of the catheter to cut or scrape out the hard plaque. The atherectomy could be Excisional (the blade cuts the plaque in one direction), Orbital (the plaque gets removed with a spinning tool), Rotational (the blade cuts the plaque in a rotating movement), or Laser ablation (the plaque is removed using laser) atherectomy.
Angioplasty – To treat any blood vessel damage, the interventional healthcare professional accesses them through minimal invasiveness. In endovascular intervention, the healthcare professional usually makes a tiny incision in the groin to gain access to the damaged arteries. Using the X-ray real-time images, the catheter, with a balloon attached, is guided to the damaged artery. Once in place, the balloon is inflated, pushing the plaque to the sides of the arterial walls, and paving the way for the uninterrupted flow of the blood.
In the case of angioplasty, the healthcare professional implants a stent, clearing the passage for the blood to flow in the affected artery. A stent, a small mesh tube, keeps the artery open for blood flow. Once the stent is placed, the balloon is deflated, the catheter is removed, and the incision is closed.
Apart from treating peripheral arteries, these stents are widely used to treat various artery blockages, like the coronary, renal, and carotid arteries.
Angioplasty has been gaining acceptance as a standard of care for treating blocked arteries due to its minimal invasiveness, resulting in less pain and tissue scarring, faster healing and recovery, shorter hospital stays, and quicker return to normalcy.
Conclusion
There are many risk factors common between PAD and heart disease; hence, effective control and management of one help to prevent the incidence of the other. PAD with other conditions of diabetes, high blood pressure, high cholesterol, or obesity puts the patient at a higher risk of heart disease. Rigorous, consistent, and aggressive lifestyle changes are a must for its prevention. However, in severe cases, where self-care, medications, lifestyle changes, and other alternate treatment modalities do not offer the desired results, surgical and non-surgical treatment options should be resorted to for timely and effective treatment.
The choice of the medical treatment option depends on the healthcare professional’s decision, arrived at after considering the severity of the condition, the age, anatomy, and overall health of the patient. Surgical and non-surgical treatment help repair the damage to the artery by removing the blockages. However, one must own responsibility toward one’s health and adhere to the doctor-recommended diet plan, exercise regime, and recovery plans, and quit smoking and tobacco consumption post-treatment for healthy living.
References
https://journals.lww.com/cmii/fulltext/2020/18030/endovascular_therapy_in_vascular_surgery___how.2.aspx#:~:text=41%E2%80%9354%20million%2C%20with%20an%20estimated%204.2%E2%80%936.2%20million%20patients%20of%20critical%20limb%20ischemia
https://www.heart.org/en/news/2023/06/15/routine-tests-may-reduce-disparities-in-peripheral-artery-disease-and-amputation-risk
https://www.narayanahealth.org/blog/what-is-peripheral-arterial-disease-pad/#:~:text=According%20to%20an%20International%20organization,built%20up%20in%20the