Peripheral Vascular Disease (PVD) is a common but an often overlooked condition that affects the blood vessels other than the heart and brain. These blood vessels carry oxygen-rich blood to your limbs, and when they’re narrowed or blocked, it can lead to serious health problems. Early diagnosis and management of PVD can make a significant difference in preventing complications and improving your quality of life. In this blog, let’s learn what PVD is, how to recognize its signs and symptoms, and ways to manage and prevent it effectively.
What is Peripheral Vascular Disease?
PVD is a condition that occurs when blood vessels in the legs, arms, or other peripheral parts of the body become narrowed or blocked. This is usually caused by the buildup of fatty deposits in the arteries, reducing blood flow. Over time, this reduced circulation can lead to pain, mobility issues, and even more severe complications like ulcers or infections.
Importance of Early Detection
Detecting PVD early is crucial for preventing its progression. When it’s in the early stages, you can usually manage it with simple lifestyle modifications and treatments. But if it progresses, it might need more serious interventions. That’s why it’s so important to know the symptoms and talk to a doctor right away. Acting quickly can lower your risk of complications and keep your vascular health in check.
Types of PVD
PVD is broadly classified into two main types:
- Functional PVD: This type is caused by spasms in the blood vessels that temporarily limit blood flow. It is often triggered by cold temperatures or stress. [2][MJ1]
- Organic PVD: This is caused by structural changes in the blood vessels, such as narrowing or blockages due to fatty deposits (atherosclerosis).
Risk Factors for PVD
Several factors can increase your risk of developing PVD, including:
- Smoking
- High blood pressure or cholesterol
- Diabetes
- Being overweight
- Lack of physical activity
- Family history of vascular disease
People over 50 years of age or those with a history of cardiovascular issues are also at higher risk.
Recognizing Early Signs and Symptoms of PVD
| Stage | Symptoms | Details to Watch For |
| Common Symptoms | Pain or cramping in the legs or hips during physical exertion, relieved with rest (claudication). | – Numbness, weakness, or a heavy feeling in the legs. – Coldness in the lower legs or feet compared to the rest of the body. |
| Subtle Early Signs | Slow-healing wounds or sores on the legs or feet. | – Change in skin color, such as pale or bluish tone. – Shiny skin or loss of hair on the affected area. |
| Advanced Symptoms | Severe pain in the legs, even at rest. | – Non-healing ulcers or infections on the feet. – Tissue damage that may require surgery or, in severe cases, amputation. |
Importance of Early Diagnosis and Screening
Who Should Get Screened?
Screening is essential for people who:
- Have a history of diabetes/family history, high blood pressure, or high cholesterol.
- Smoke or have smoked in the past.
- Experience symptoms like leg pain or non-healing wounds.
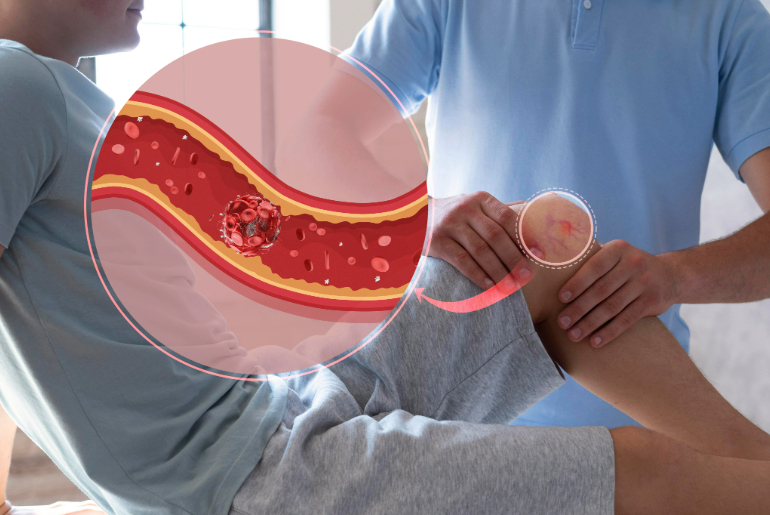
Diagnostic Tests for PVD
When it comes to diagnosing PVD, doctors have a few key tools to figure out what’s going on. One common test is the Ankle-Brachial Index (ABI), which compares the blood pressure in your ankle and arm to spot any reduced blood flow. [5][MJ1] They might also use an ultrasound, which uses sound waves to get a clear picture of how blood is flowing in your arteries/veins. If more detail is needed, there’s angiography, an imaging with a diagnostic test that pinpoints blockages in your blood vessels.
Getting screened early makes a huge difference—it allows doctors to create a personalized treatment plan to keep the condition under control.
Management and Treatment Options for PVD
Managing PVD involves a combination of lifestyle modifications, medications, and, in some cases, medical procedures.
- Lifestyle Modifications:
- Quit smoking to improve blood circulation.
- Adopt a healthy diet rich in fruits, vegetables, and whole grains to reduce cholesterol.
- Engage in regular physical activity, such as walking, to improve blood flow.
- Medications:
In some cases, medications may be prescribed to manage symptoms or reduce the risk of progression of the disease.
- Medical Procedures:
For severe cases, interventions like angioplasty (widening of the artery) or bypass surgery may be recommended to restore blood flow.
Preventive Measures to Protect Vascular Health
Prevention is key to maintaining healthy blood vessels. Here are some tips to protect your vascular health:
- Stay Physically Active: Regular exercise helps improve circulation and strengthens your heart.
- Eat a Balanced Diet: Focus on foods low in saturated fats and high in fiber to reduce the risk of atherosclerosis.
- Monitor Your Health: Keep your blood pressure, cholesterol, and blood sugar levels under control.
- Avoid Smoking: Smoking damages blood vessels and significantly increases the risk of PVD.
Taking these steps early in life can greatly reduce your chances of developing PVD and other vascular issues.
When to Seek Medical Help
It’s important to consult a doctor if you experience:
- Persistent leg pain during activities that improves with rest.
- Non-healing sores or wounds on your feet.
- Unexplained numbness, weakness, or coldness in the legs.
- Sudden and severe leg pain accompanied by swelling or discolouration.
Timely medical attention can prevent complications and ensure the best possible outcomes for your vascular health.
Conclusion
Peripheral Vascular Disease is a serious but manageable condition when detected early. By recognizing the symptoms, understanding the risk factors, and adopting healthy lifestyle habits, you can protect your vascular health and improve your quality of life.
Don’t ignore signs like leg pain or slow-healing wounds—these could be your body’s way of signaling a vascular issue.
References:
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/peripheral-vascular-disease#:~:text=Peripheral%20vascular%20disease%20(PVD)%20is,%2C%20veins%2C%20or%20lymphatic%20vessels.
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/peripheral-vascular-disease#:~:text=Peripheral%20vascular%20disease%20(PVD)%20is,%2C%20veins%2C%20or%20lymphatic%20vessels.
- https://vascularsurgery.wustl.edu/patient-care/peripheral-vascular-disease/#:~:text=Organic%20PVD%20is%20caused%20by,that%20block%20normal%20blood%20flow.
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/peripheral-vascular-disease#:~:text=temperatures%20or%20stress.-,Risk%20factors%20of%20peripheral%20vascular%20disease,High%20blood%20cholesterol%20(hypercholesterolaemia).,-Diagnosis%20of%20peripheral
- https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/ankle-brachial-index-test#:~:text=The%20ankle%20brachial%20index%2C%20or,The%20result%20is%20the%20ABI.