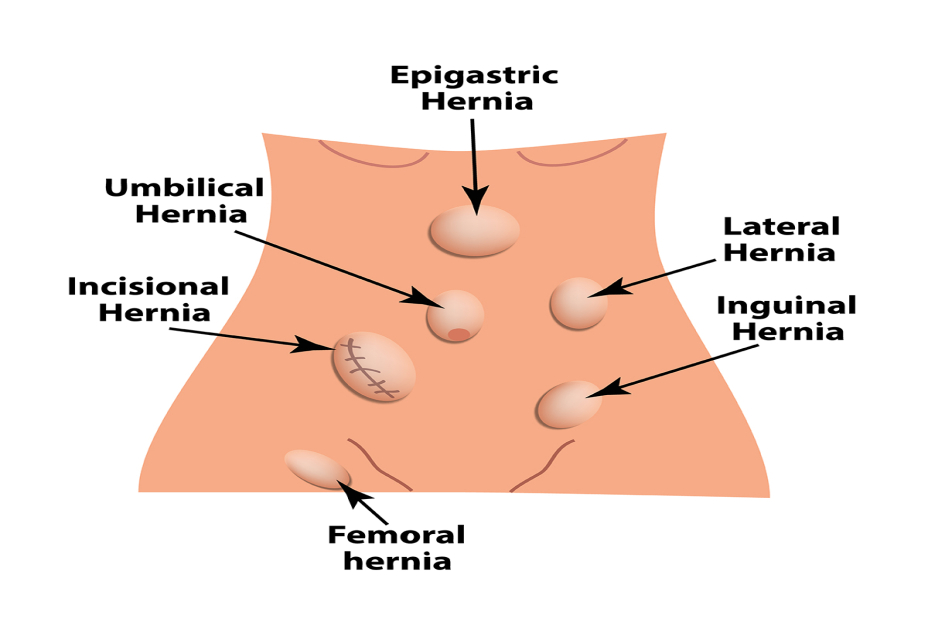
Considering a hernia surgery? Let’s take you through this article that will help you explore different treatment options for a hernia surgery.
Hernias do not heal on their own. Though they can remain asymptomatic for a long time and cause no trouble, they also have high possibilities of getting worse with time. Usually surgical repair is recommended for treating hernias but your doctor may prescribe OTC (Over-the-Counter) antacid medicines at times to reduce the risk of your hernia or may ask you to wear a supporting truss. It is important to understand that hernias in most cases are not immediately life-threatening but it does require treatment as they normally do not get better on their own. Apart from an umbilical hernia in infants, the nature of treating a hernia normally depends on symptom presence. If an adult has the same, surgery is usually recommended because the complications are most likely to increase with time.
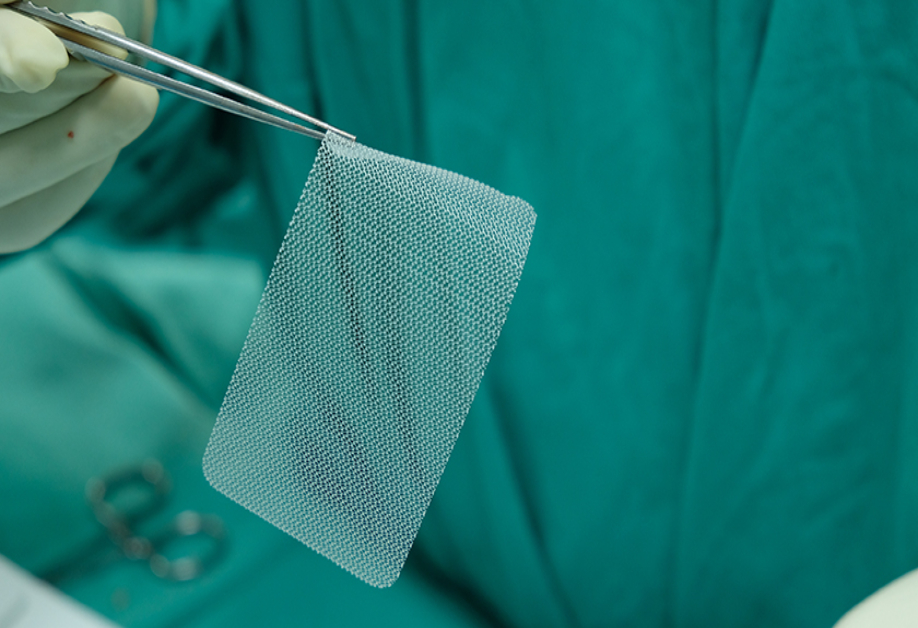
As per available evidence, surgical repair is the only current effective way to treat a hernia. To prevent the hernia surgery is performed to return bulging tissue to its proper place, and then repair the defect in the abdomen with stitches or a mesh patch. There are generally two types of a hernia surgery- open repair and laparoscopic repair.
1) Open Hernia Repair
A single long incision is made in the groin area for this kind of repair. The weak spot in the muscle wall is then fixed by sewing the edges of healthy muscle tissues collectively for the contents to be pushed back into the abdominal cavity. This approach is suitable for more diminutive hernias that may have been present since birth, and for healthy tissues without addressing stress on the tissue. This type of surgery can be performed under general, spinal, and local anesthesia.
What to expect after the open hernia surgery?
- In most of the cases, patients are able to go home the same day. However, recovery time is usually about 3-4 weeks.
- You can most likely return to performing light activities after 3 weeks.
- Strenuous tasks must wait until after 6 months of recovery.
- Avoid tasks that may cause severe pain.
2) Laparoscopic Hernia Repair
Laparoscopic hernia repair uses a laparoscope, a thin, telescope-like instrument that is inserted through a small incision at the umbilicus (belly button). This procedure is usually performed under general anesthesia and before the surgery, you will have an evaluation of your general state of health and an electrocardiogram (EKG). The laparoscope is connected to a tiny video camera that projects an “inside view” of your body onto television screens in the operating room. After the procedure is completed, the small abdominal incisions are closed with the help of stitches or surgical tapes.
What to expect after a laparoscopic hernia surgery?
- In most of the cases, patients are able to go home the same day itself however, recovery time is usually about 1-2 weeks.
- You can most likely return to performing light activities after 1-2 weeks.
- Strenuous tasks must wait until after 4 months of recovery.
- Avoid tasks that may cause severe pain.
Recent studies have revealed that in the short term, laparoscopic repair is superior to open repair in terms of less blood loss, fewer operative complications, and shorter hospital stay. Long-term outcomes such as recurrence rates are yet unexplained. However, a hernia can reoccur even after the surgery. And, which is why patients are advised to adapt a healthy lifestyle post a hernia surgery. While not much can be done to prevent muscle weakness, one can reduce pressure on the abdomen, and thus reduce the risk of incurring a hernia. Maintaining a healthy body weight can reduce the risk of getting a hernia as your extra body fat can put pressure on your abdomen. Likewise quitting smoking, avoiding lifting of heavy objects can also help in reducing the risk of getting a hernia. Also, staying aware of any symptoms is the key to identifying and treating a hernia on time. It is important to keep in mind that hernias do not go away on their own and will need medical attention at some point of time.