Chronic sinusitis is an illness that causes inflammation of the lining of the nose and the sinuses. Symptoms of chronic sinusitis include facial pressure, nasal congestion, discolored nasal discharge, and post-nasal drip. The majority of the patients with chronic sinusitis can be treated with medication. However, for a small percentage of patients, infections recur and may persist for a longer course even after medication. Such patients benefit from surgery. After reviewing your medical history and x-ray studies, your ENT specialist can determine if surgery is needed.
What is balloon Sinuplasty?
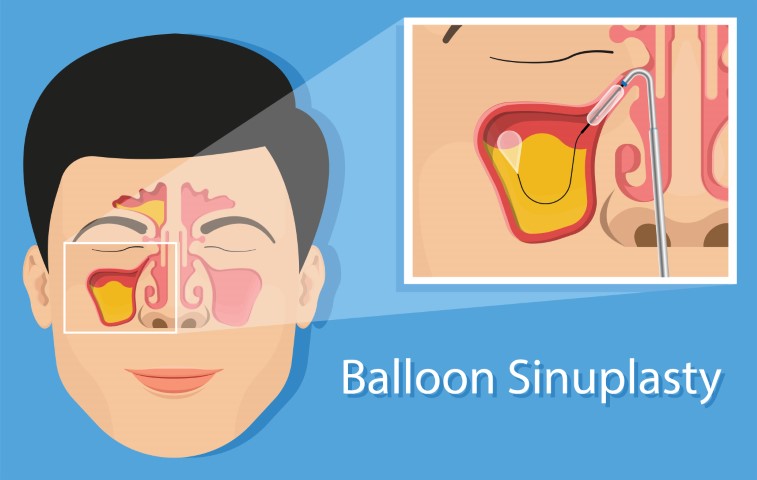
Balloon sinuplasty is also known as balloon catheter dilation surgery or “smart sinus” procedure. It is a relatively new surgery and is a procedure to clear blocked sinuses. It has been approved by the Food and Drug Administration in 2005.
Balloon Sinuplasty was adapted from angioplasty, a procedure in which balloon catheters are used to dilate congested blood vessels near the heart.
The complications of the procedure are reportedly minimal and the recovery period is quite short. While the procedure is minimally invasive, it is still a surgery and it carries the kind of risks of a few side effects.
How does Balloon Sinuplasty work?
Most people who need the surgery have a condition that results in the sinus membranes becoming inflamed, preventing drainage of mucus, pus, and discharge, and causing congestion. Over time, blockage and inflammation in the nasal passages can cause symptoms, such as a headache, jaw ache, and even insomnia.
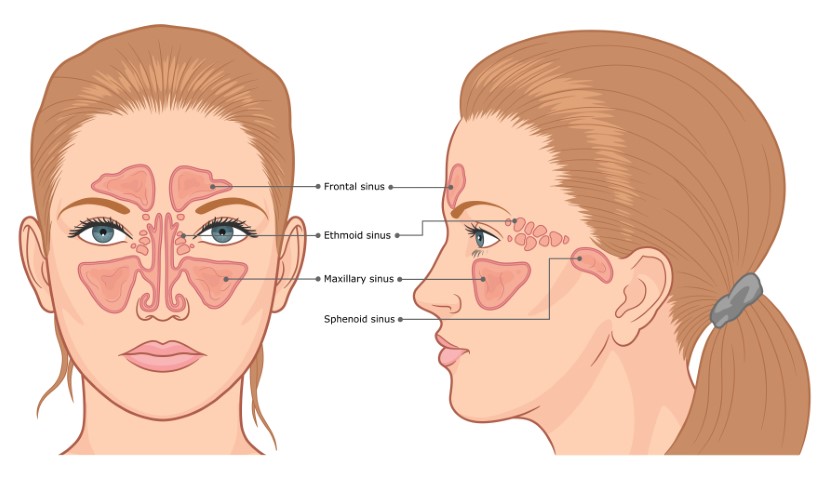
Balloon sinuplasty allows the openings of some or all three of the major nasal sinuses to be dilated. The doctors widen the blocked nasal passages by flushing out or remove congestion, often by using a saline solution.
This helps them to be cleared and drained. Balloon sinuplasty uses small balloon catheters that inflate to drain the large nasal sinuses and is typically used to treat cases of severe rhinosinusitis or sinus inflammation and blockage in the nose.
What does the balloon sinuplasty procedure include?
Depending on individual factors and preferences, balloon sinuplasty is done by an ear, nose, and throat (ENT) doctor in their office, clinic, or a hospital.
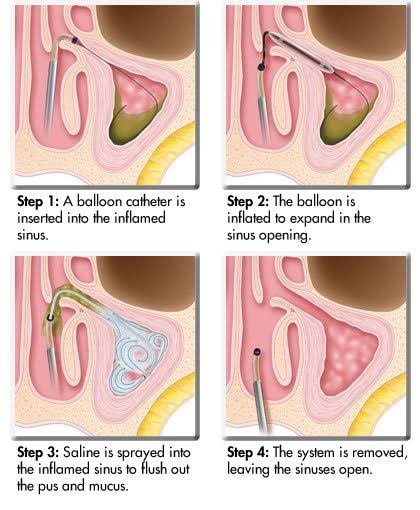
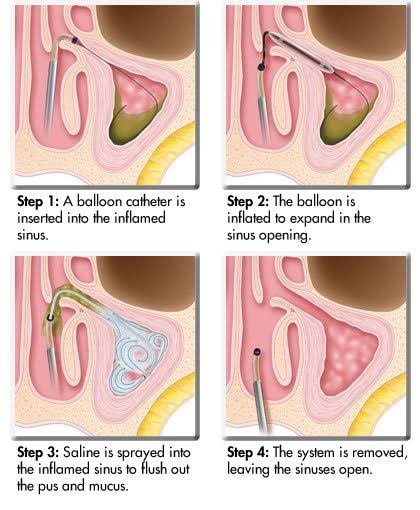
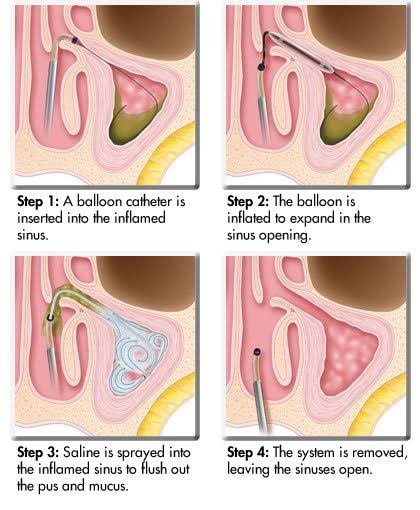
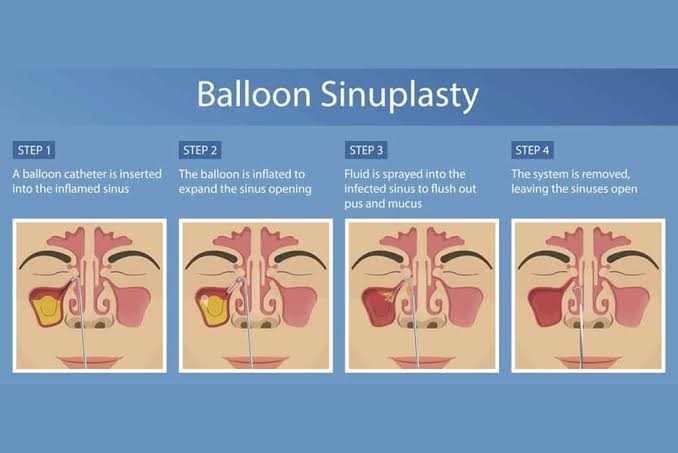
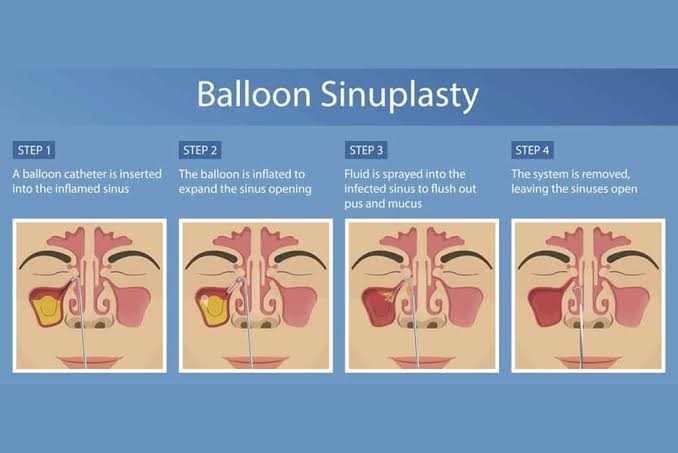
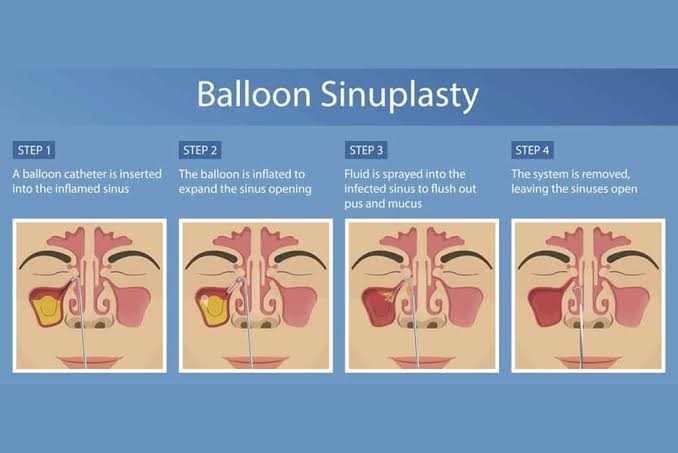
After administering a local or general anesthesia, a doctor inserts an endoscope, a thin, flexible plastic tube with a camera and light on the end, into the nasal passages. On reaching the entrance to the cavity, a small balloon catheter is advanced over the guiding endoscope wire.
The balloon is then slowly inflated and pressed against the sinus walls, once it is positioned inside the nasal passage and cavity. This is done to fracture the bone slightly and force an opening. Once the balloon is fully inflated, the cavities and passageways are flushed out using a saline rinse, and debris is further removed. Once the balloon is removed the sinus is allowed to continue to drain naturally.
Most people who undergo balloon sinuplasty have reported feelings of numbness or sinus pressure only during the surgery. Any noticeable pain is not reported.
Advantages of Balloon Sinuplasty over traditional methods
Endoscopic sinus surgery is a procedure to open the natural drainage pathways of the sinuses to restore their independent function. Endoscopic surgery comes with its risks and complications such as bleeding, recurrence of disease, spinal fluid leak, visual issues, etc.
Benefits of balloon sinuplasty over traditional endoscopic sinus surgery
- There is a lower risk of bleeding
- Faster recovery
- Since there isn’t any removal of sinus tissues, structures, bones, or sinus cartilage, there is no intended damage
- Fewer required post-operative sessions
- Fewer medications required during and post-operation
- reduced risk of scarring and continued inflammation
What happens after the surgery?
Usually, sinuplasty tends to have minimal side effects. However, most people can go home a few hours after the surgery is complete and return to normal activities in a day or two.
Some common side effects of Balloon Sinuplasty
- Bloody drainage for a few days
- Nasal, cheek, or forehead tenderness
- Minor swelling in the nasal cavities and passages
- Minor swelling in the surrounding facial area
- congestion
- Failure to properly cleanse the sinuses after the surgery can sometimes cause infection
Regardless of these minor side effects, Balloon sinuplasty is considered a very safe and effective procedure. After it was first introduced in the mid-2000s, balloon sinuplasty has become one of the most commonly performed types of sinus surgeries. It gains its popularity by being associated with high rates of success and low risks or complications.
A study conducted in 2016 found that all 15 adults who received balloon sinuplasty reported improved symptoms 3-6 months post-surgery, without any unanticipated complications or side effects. Similarly, a study done in 2017 found that balloon sinuplasty was successful in treating 94 percent of chronic sinusitis in 30 children who underwent the surgery. The positive effects persisted even a year post-surgery.