Want to adopt a heart-healthy diet post angioplasty, but aren’t sure where to start?
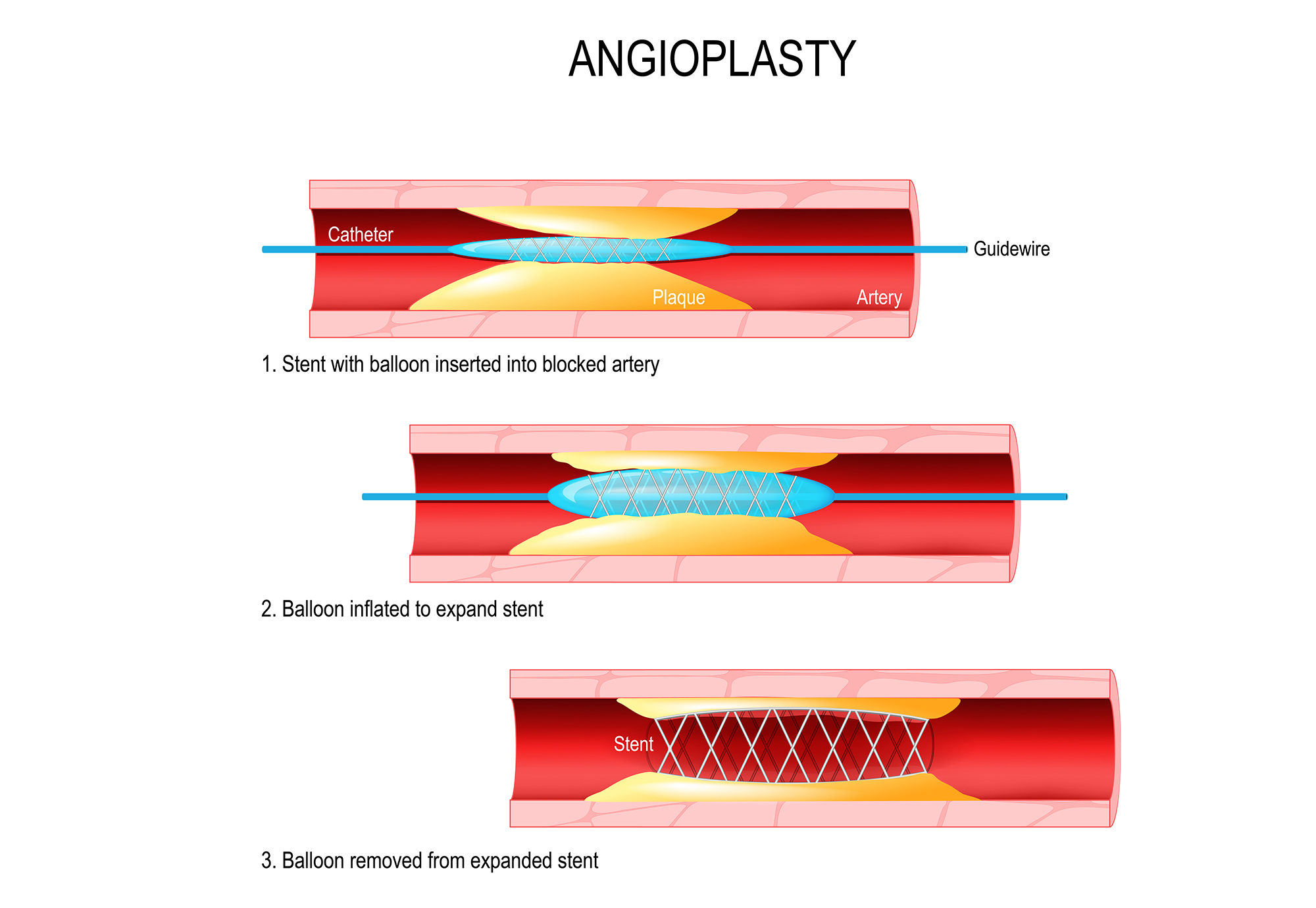
One way to begin is by giving a complete makeover to your current diet plan. Focus on making meal plans that emphasize vegetables, fruits and other necessary products with an adequate amount of proteins, carbohydrates and other nutrients. We know, that the main question here is about what exactly to consume and what to avoid post implanting a stent as you may not be that well versed with every food category and ingredients benefiting a person. Hence, we have stated below foods to intake and to avoid after implanting a stent.
Firstly, it is very important that you consult a doctor before jumping onto conclusions and making your diet plans, especially after angioplasty. It is important to understand that each one of us is built differently and one particular diet plan isn’t going to work for all of us. And, hence we believe that even minor differences in your diet post angioplasty can make a huge difference to your heart health. Now, let us read more about it.
- Consume more whole-grain foods every day: Eating whole grains is associated with various benefits, including a lower risk of diabetes, heart disease, and high blood pressure. They are rich in nutrients, minerals, fibers, antioxidants and has also proven to reduce the risk of a heart attack.
- Eat more quantities and varieties of fruits and vegetables: People who eat more vegetables and fruits as part of an overall healthy diet are likely to have a reduced risk of some chronic diseases like stroke, cancer, diabetes, influenza or any respiratory disease. They provide nutrients vital for health and maintenance of your body.



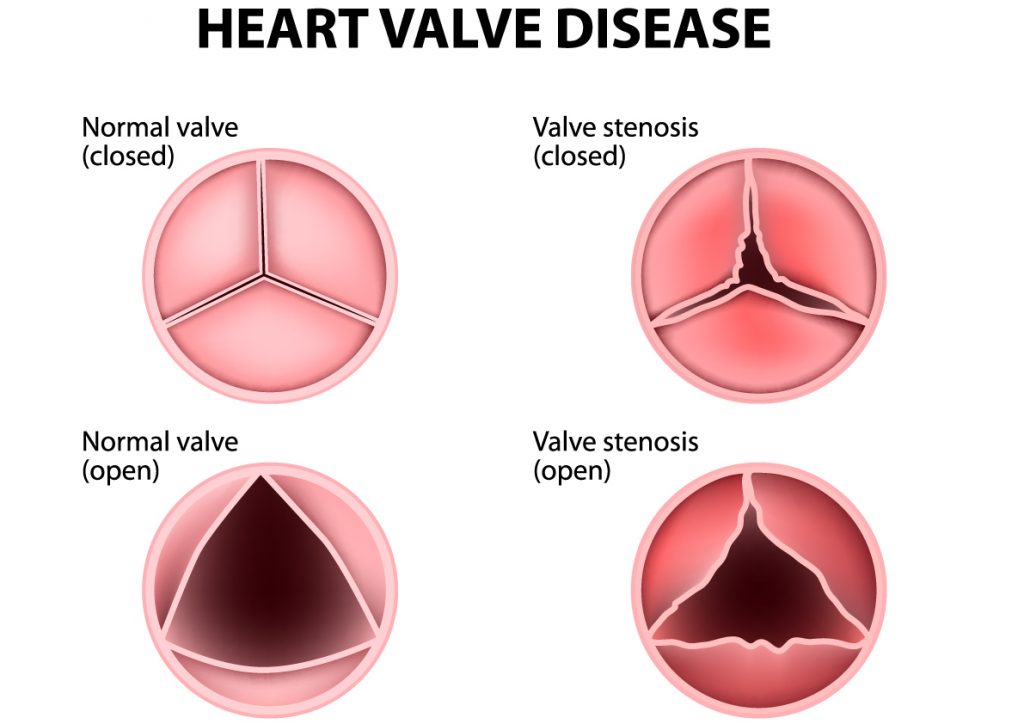
- Reduce salt and sugar intake: Salt and sugar are needed for health. However, we require very little of it to survive. While salt is essential for the transmission of nerve impulses and normal cell function, sugar is a real source of energy with glucose being the most important of all. But, due to rapid urbanization and changing lifestyles, dietary patterns have seen a major shift and processed foods are being consumed more which is indirectly increasing the risk of heart diseases and strokes due to the high amount of salt and sugar content in it. And, for a person who has just undergone Angioplasty, it becomes highly important to maintain a healthy balance of salt and sugar to avoid any further heart illnesses.
- Cut down on the consumption of fatty foods, rich in LDL, trans fats and saturated fats: Eliminate fatty meats like pork, lamb or fried items, butter, or coconut oil from your diet. There are two main types of potentially harmful dietary fats, trans fat and saturated fat. These types come mainly from animal sources of food, such as red meat, poultry and full-fat dairy products especially whole milk. They raise high-density lipoprotein (HDL or “good”) cholesterol and low-density lipoprotein (LDL or “bad”) cholesterol levels, which may increase your risk of cardiovascular disease.
- Include good fats in your diet: Dietary fats are important for your body as it is responsible for supplying energy and to support cell growth. They also help in protecting your organs and help in absorbing nutrients and produce important hormones. The simplest way to differentiate good and bad fats is, good fats remain in liquid form at room temperature. Monounsaturated fats and polyunsaturated fats are known as “good fats” because they are good for your heart, cholesterol, and overall health. Some of these sources are nuts, olives, flax seeds, fish oils, etc. Bad fats are of two types, Saturated fat and Trans fat and these have been identified as potentially harmful to your health. Most of the foods that contain these types of fats are solid at room temperatures, such as butter, coconut/palm oil, margarine, beef or pork fat, etc.



- Fish and lean meat are good options for individuals taking non-vegetarian meals: Lean meats and fish have relatively low-fat content and have high amounts of protein. Protein is an essential part of a balanced diet. Beyond protein’s essential roles in building and maintaining muscle and tissues in your body and helping regulate many body processes, it also promotes satiety fullness and may help in managing your weight.
- Avoid consumption of red meat: Red meats (beef, pork and lamb) have more saturated (bad) fat than chicken, fish and vegetable proteins such as beans. Saturated and trans fats can raise blood cholesterol and make heart diseases worse.
Finally, remember that a healthy diet is a mixture of all foods you eat and not only power foods that you think are filled with necessary nutrients. Having the right mix of everything (protein, fats, carbohydrates and other nutrients) after Angioplasty is always regarded as healthy. So, speak to your cardiologist, get expert advice on it and work towards building meals that are aimed towards a better and faster recovery.