What is Sinusitis?
Sinusitis/Rhinosinusitis is an infection or inflammation of the tissues lining the sinuses. It leads to poor or blocked sinus drainage. Sinusitis can occur in people of any age. Sinusitis in children also often & cause discomfort to the patient.
What are the symptoms of Sinusitis?
According to the American Academy of Otolaryngology-Head and Neck Surgery, the signs of sinusitis include:
- Nasal inflammation
- Nasal obstruction or Congestion
- Pain, tenderness, and swelling around the eyes, cheeks, forehead, nose
- Continuous Headaches
- Runny nose
- Thick & discolored discharge from the nose
- Allergies & nasal polyps lead to sinus pain and symptoms
- Loss of smell and taste, and infections
Worldwide sinusitis affects millions of people every year.
Acute vs. Chronic
Acute sinusitis lasts for a short period, as stated by the American Academy of Otolaryngology. It’s less than four weeks. During an Acute sinus infection, the patient suffers from a cold attack or other respiratory illness.
Chronic sinus infections last for more than twelve weeks. It may recur periodically. Allergies & nasal polyps are commonly noticed in these patients.
Sinusitis in Children
Sinusitis in children is a concern, and parents need to consider it seriously & check-up with their doctor. The child’s nose needs to be examined to determine the cause of sinusitis. A mucus sample of the child may show what germ is causing the infection. It can help the doctor to opt for the appropriate treatment. Even if the child’s symptoms go away on their own, the recurring sinus attack history should be reported to the doctor’s attention. Immune problems or antibody deficiencies may be risky for chronic sinusitis.
What causes sinusitis in a child?
When the sinuses are blocked due to the infection, bacteria may start to grow. This leads to sinusitis or Nasal Congestion
The most common bacteria that cause acute sinusitis include:
- Moraxella catarrhalis
- Streptococcus pneumonia
- Haemophilus influenzae
How is sinusitis diagnosed in a child?
The Doctor will record the Medical health history of the child and ask for a physical exam. The child may have tests, such as:
- Sinus X-rays: An X-ray exam of the sinuses may help with the diagnosis.
- CT scan of the sinuses: A CT scan shows detailed images of the sinuses
- Cultures from the sinuses: A swab of discharge from the nose may be taken. The sample is checked for the culture of bacteria or other germs.
What are the treatments available for Sinusitis?
The ENT specialist will be the best option to treat sinusitis in a child with pain relievers, antibiotics, allergy medications, decongestants, or steroids.
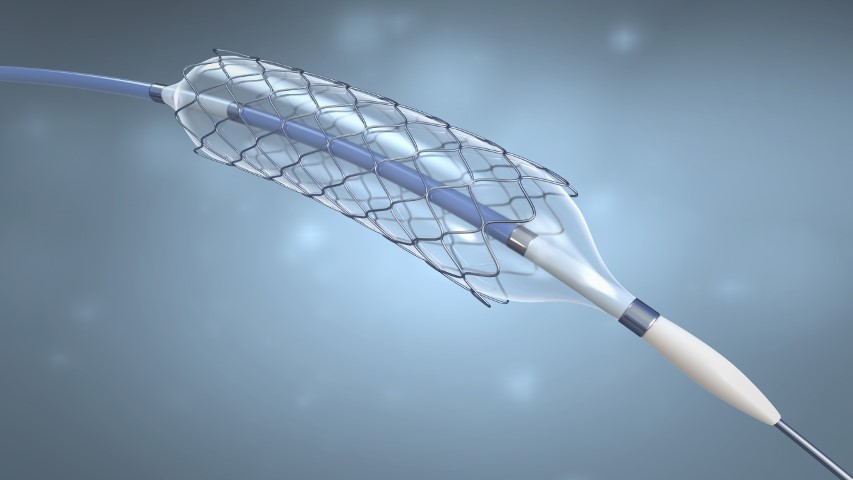
According to Ann Otol Rhinol Laryngol 2009 March, Balloon Sinus Dilation Procedure in children seems to be very encouraging. There is no bone or tissue removal, the procedure seems to be suitable for use in children.
Safety and feasibility of Balloon Sinus Dilation Procedure for treatment of chronic rhinosinusitis in children
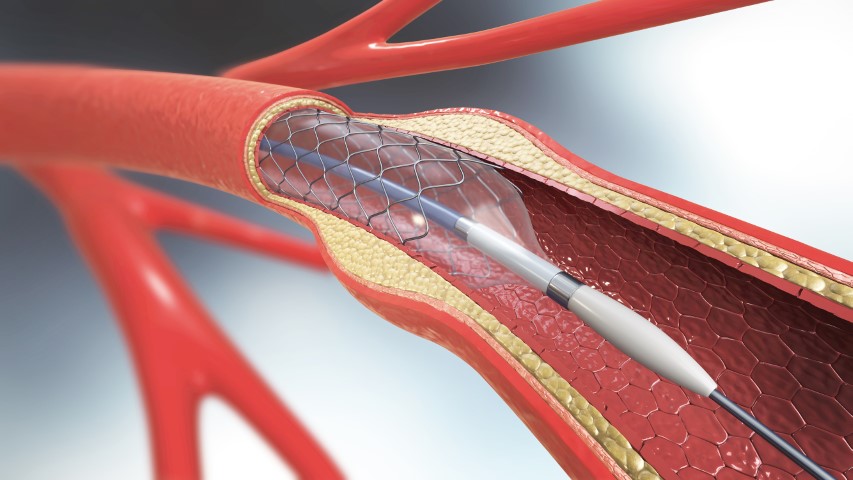
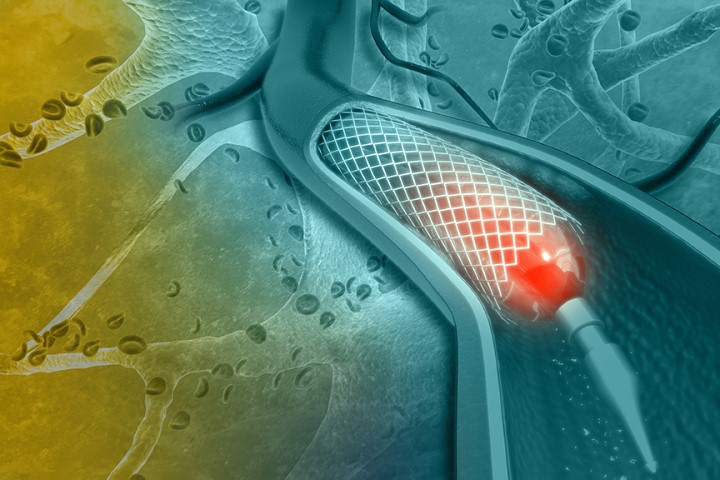
Balloon Sinus Dilation Procedure can treat chronic rhinosinusitis (CRS) by opening your blocked sinuses & you will get relief. This technique allows for restoring ventilation to the sinuses with minimal trauma to the tissues. According to Am J Rhinol Allergy Jan-Feb 2010, Balloon Sinus Dilation Procedure of the sinus Ostia in children was safe and a significant number showed improvement.
Here are some benefits of the Balloon Sinus Dilation Procedure:
1. This is a minimally invasive procedure
The Balloon Sinus Dilation Procedure doesn’t need an incision. The balloon is inflated to open the sinus passage, the cavity is cleaned and drained. No incisions or stitches are necessary.
2. The procedure takes very little time
The Balloon Sinus Dilation Procedure can be performed in the ENT’s office or OT, and it takes about an hour.
3. Faster Recovery
Minimally invasive procedures provide faster recovery compared to traditional surgery ― and Balloon Sinus Dilation Procedure is no exception. The majority of patients return to their normal activities within a couple of days.
4. No nasal packing
Traditional nasal surgeries require nasal packing for absorbing the bleeding. Remember, there’s no need for incisions or bone/tissue removal with Balloon Sinus Dilation Procedure, so you will not experience the same post-surgical discomfort.
5. Long-lasting relief
The most rewarding benefit of a Balloon Sinus Dilation Procedure is, the relief is Long-lasting. In a research article published in the journal Otolaryngology-Head and Neck Surgery, patients report relief for up to two years after the procedure.
Talk To The ENT
If your child has chronic rhinosinusitis (CRS), it’s time to talk to the ENT. Make an appointment to discuss and find out if a Balloon Sinus Dilation Procedure is the best option for your child. Your child will recover soon if he or she gets the proper treatment from an ENT.