Lung cancer is the most common cancer in the world. According to the World Health Organization, there were 2.21 million cases in the year 2020. It is the most common cause of death around the world. Patients have a 13 times better chance of living for five years if they are diagnosed early. Lung Cancer Awareness Month (LCAM) is celebrated every year in November to raise awareness about the disease and continue to challenge the stigma associated with lung cancer.
The goal of the month is to urge individuals to seek medical assistance sooner rather than later, to encourage early diagnosis so that patients have the best chance of a successful treatment, and to emphasise other key aspects that affect patient outcomes. Educating people on the complexity of lung cancer, the vast spectrum of people who are affected, and the harmful effects of lung cancer stigma can aid in earlier diagnosis and better patient treatment. Furthermore, LCAM is also an occasion to highlight therapeutic developments, advocate for global access to care, and, most importantly, demonstrate our support for patients and their loved ones.
Facing the stigma
Lung cancer is often misunderstood to be solely a smoker’s disease. However, more than half of individuals diagnosed are former smokers or non-smokers. This misunderstanding has been associated with poor outcomes due to factors like waiting too long to seek treatment, disease-related distress, a lack of social support, and poor care quality.
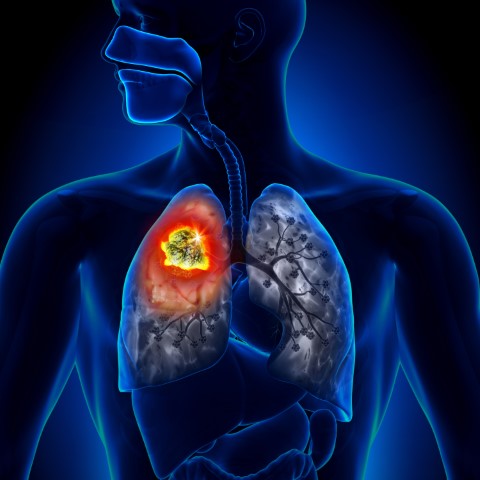
What you need to know about Lung cancer
Cancer is a condition in which the cells of the body grow out of control. Lung cancer is cancer that starts in the lungs and spreads throughout the body. Lung cancer begins in the lungs and can spread to the lymph nodes or other organs in the body, including the brain. Cancer that has spread to other organs may extend to the lungs as well. Metastases are the spread of cancer cells from one organ to another.
There are two types of lung cancer:
Small cell lung cancers (SCLC) and non-small cell lung cancers (NSCLC) are the two forms of lung cancer. This classification is based on the appearance of tumour cells under a microscope. Making the distinction between these two types of tumours is critical since they develop, spread, and are treated differently.
SCLC accounts for roughly 10% to 15% of all lung malignancies. This form of lung cancer is the most aggressive and fastest-growing of all. Cigarette smoking is highly linked to SCLC. SCLCs spread quickly throughout the body, and they are usually detected after they have spread widely.
The most common type of lung cancer is non-small cell lung cancer (NSCLC), which accounts for roughly 85% of all occurrences. NSCLC is divided into three categories based on the cells detected in the tumour. They are as follows:
- Adenocarcinomas, like other lung cancers, are linked to smoking, this form is also seen in nonsmokers, particularly women, who get lung cancer. The majority of adenocarcinomas develop in the lungs’ periphery. They have a proclivity for spreading to lymph nodes and beyond.
- Squamous cell carcinomas used to be more common than adenocarcinomas, but now they make up around 25% to 30% of all lung cancer cases. Squamous cell tumours are most common in the bronchi of the central chest. This type of lung cancer tends to stay in the lung, spread to lymph nodes, and grow large enough to produce a cavity.
- Large cell carcinomas, also known as undifferentiated carcinomas, are the least prevalent kind of NSCLC, accounting for 10% to 15% of all lung cancer cases. This malignancy has a significant proclivity for spreading to lymph nodes and distant locations.
- Adenocarcinomas, like other lung cancers, are linked to smoking, this form is also seen in nonsmokers, particularly women, who get lung cancer. The majority of adenocarcinomas develop in the lungs’ periphery. They have a proclivity for spreading to lymph nodes and beyond.
- Squamous cell carcinomas used to be more common than adenocarcinomas, but now they make up around 25% to 30% of all lung cancer cases. Squamous cell tumours are most common in the bronchi of the central chest. This type of lung cancer tends to stay in the lung, spread to lymph nodes, and grow large enough to produce a cavity.
- Large cell carcinomas, also known as undifferentiated carcinomas, are the least prevalent kind of NSCLC, accounting for 10% to 15% of all lung cancer cases. This malignancy has a significant proclivity for spreading to lymph nodes and distant locations.



Types of Treatment
Depending on the type of lung cancer and how far it has gone, there are numerous treatment options. Surgery, chemotherapy, radiation therapy, targeted therapy, or a combination of these treatments can be used to treat non-small cell lung cancer. Small cell lung cancer is usually treated with a combination of radiation and chemotherapy.
- Surgery: A procedure in which surgeons remove cancerous tissue from the body.
- Chemotherapy: Special medications are used to shrink or kill cancer cells. The drugs can be pills that you consume or medicines that are injected into your veins, or both.
- Radiation therapy: Treatment that involves the use of to kill cancer, high-energy rays (similar to X-rays) are used.
- Target therapy: Drugs are used to stop cancer cells from growing and spreading. The drugs can be taken orally or administered intravenously. Before targeted therapy is employed, tests will be performed to determine if it is appropriate for your cancer type.
In the treatment of lung cancer, doctors from various specialties frequently collaborate. Pulmonologists are doctors who specialise in lung illnesses. Surgeons are medical professionals who carry out procedures. Thoracic surgeons specialise in surgery of the chest, heart, and lungs. Medical oncologists are doctors who specialise in using medications to treat cancer. Radiation oncologists are doctors who use radiation to treat cancer.
It is important to educate yourself and your loved ones about the most common type of cancer so that lives can be saved. If you notice anything unusual contact your doctor immediately.