We have all heard the story. A relative or an acquaintance experiences chest pain and immediately rushes to the hospital only to find out that it was severe gas. A more morbid one has the relative ignore the chest pain as gas till it intensifies and upon being rushed to the hospital is found to have suffered a severe heart attack. All these stories underscore the symptomatic similarity between heartburn and heart attack but the truth is that while both are chest pains; they do differ in how they manifest and in symptoms. In fact, 50% of heartburns are mistaken for heart attacks in Emergency Rooms.



So what does one do when faced with debilitating chest pain? The first thing to do is calm down and figure out one’s symptoms.
Classic symptoms of heartburn are:
- A burning sensation in the breastbone or lower part of the chest or in the upper part of the stomach



- Radiating pain towards your throat instead of shoulders and arms



- Feeling of regurgitation or food coming back into your mouth or a bitter taste.



- Worsening pain when lying in a prone position



- Occurring after a heavy meal



Heart attacks, on the other hand, exhibit the following symptoms:
- Chest pain that feels like pressure, squeezing, tightness or heaviness
- The pain comes in waves and continues only for a few minutes at a time
- Felt in the central or central left of the chest and radiates to the arms, neck, jaw or back
- Accompanied by cold sweat, shortness of breath, nausea, vomiting, fatigue and dizziness.



It is advisable to rush to the doctor if these symptoms occur for more than 15 minutes. Unfortunately, not all heart attacks are accompanied by symptoms or if present are mild. Sometimes heart pain is not always a heart attack but simple heart pain or angina. In any case, any pain that is accompanied by the above symptoms warrants an immediate visit to the hospital.
The first hour after a heart attack is crucial for long term
recovery and better outcomes.
Think you have had a heart attack? There are some things that you should do at home before rushing to the hospital or while waiting for the ambulance. They are:
- Immediately consume aspirin, unless allergic to the same. This will thin your blood and prevent further clotting.



- If prescribed, then take a dose of nitroglycerin



- Ask someone knowledgeable with CPR to begin the same and start chest compressions
- Use an Automatic External Defibrillator (AED) if one is
available on hand.
While these methods may better your chances of survival and long term recovery in case of a heart attack, they will not prevent one. The best ways to prevent a heart attack are:
- Avoiding smoking, both firsthand and secondhand
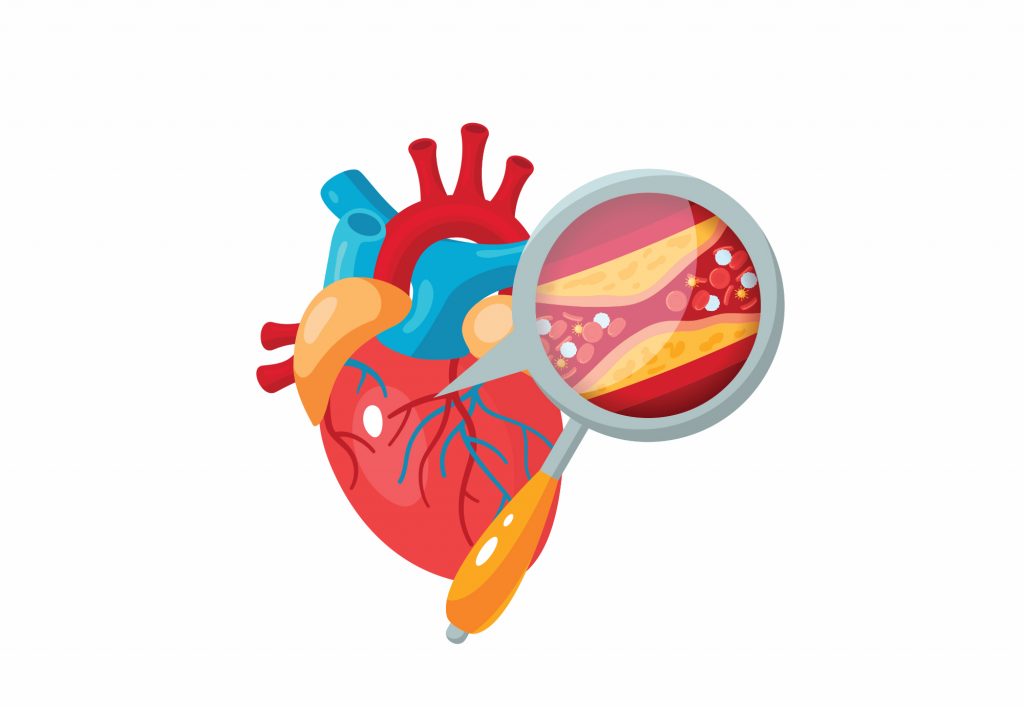
- Keeping your BP and cholesterol levels under control. This can be accomplished with dietary and lifestyle changes. Consult your doctor if you require medications for the same and remember to take them regularly.
- Go for regular health check-ups as the factors that contribute to heart disease, like high BP, cholesterol etc are usually asymptomatic in the early stages.
- Include regular physical activity. Even something as light as 30 minutes of walking, 5 times a week can go a long way in improving and maintaining your cardiac health while also keeping your weight in check.
- Reduce stress and take up hobbies that help you relieve the stress of your work and personal life.
- Consume alcohol only in moderate quantities.



Maintaining a healthy lifestyle is not only important for your cardiac health, but it is also a great way to prevent heartburn as well. Be aware of your body and don’t hesitate to go to the hospital if you are feeling any severe chest pain or accompanying symptoms. After all, it is better to be safe than sorry.