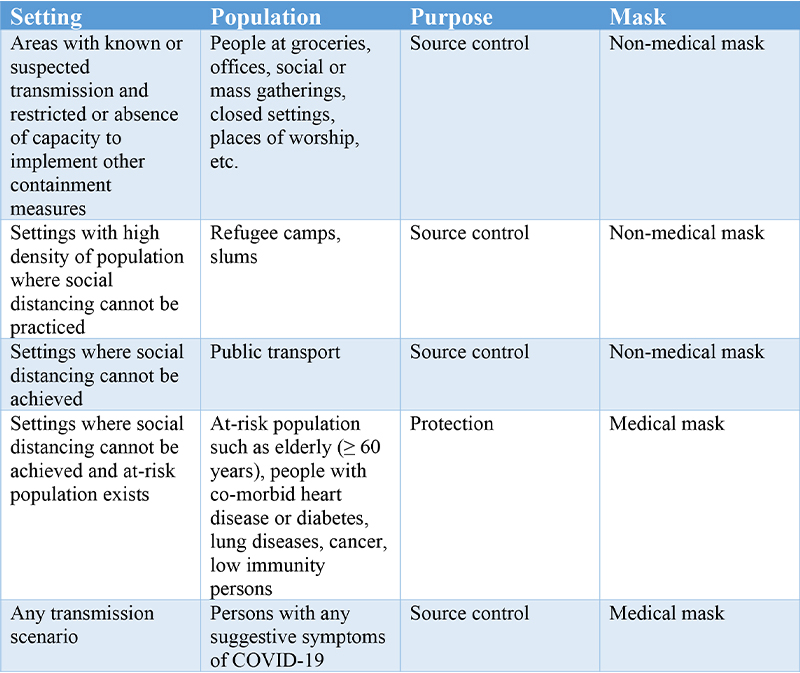
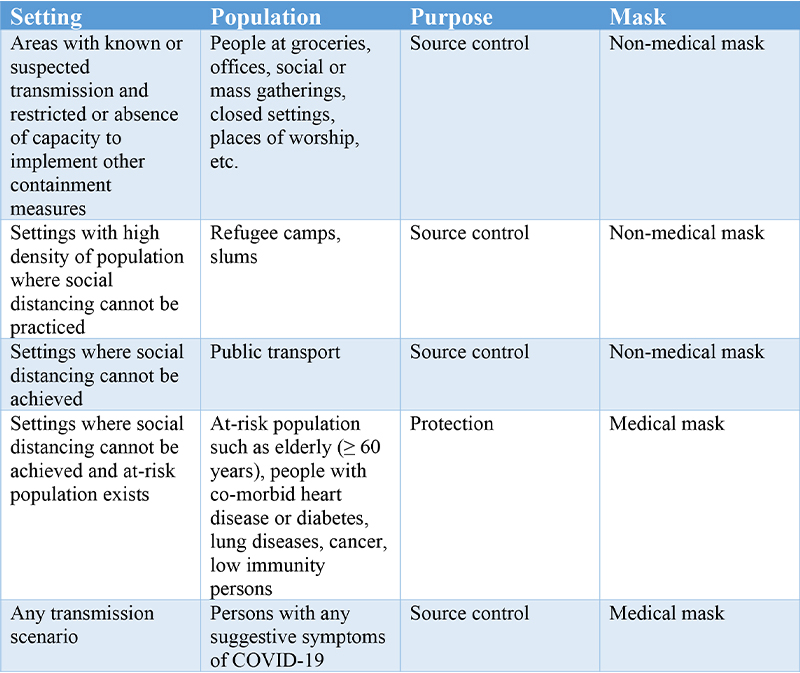
Wearing face masks is just a part of an inclusive strategy for preventing and controlling the spread of viral infectious diseases, including COVID-19. Masks can be worn by healthy persons (for self-protection while accidentally coming in contact with an infected patient) or by an already infected patient for preventing further spread of the infection (source control). But, solely using a mask cannot provide optimum protection or source control. The WHO advises people to wear masks when unable to maintain social distancing. Compliance to other infection prevention and control (IPC) measures, such as maintaining social distancing and practicing hand hygiene are imperative to prevent human transmission of the viral disease.
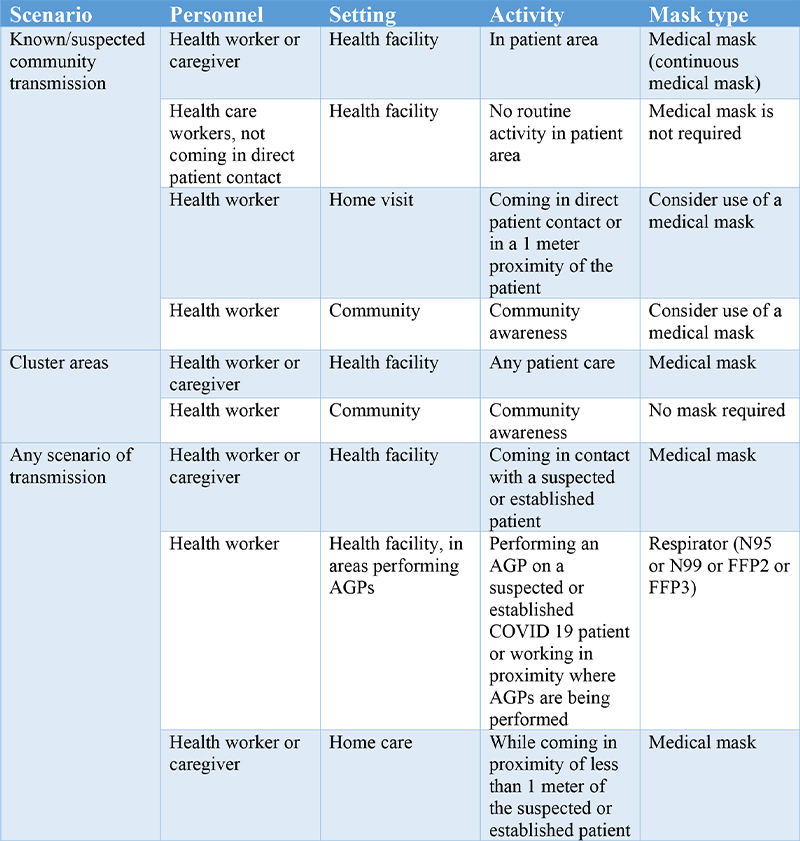
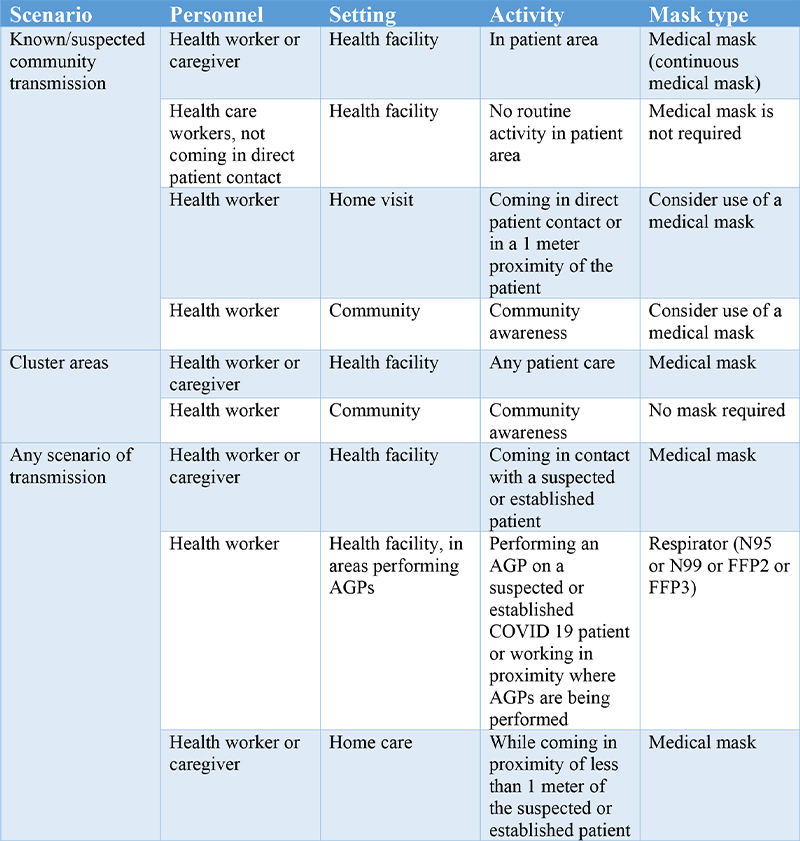
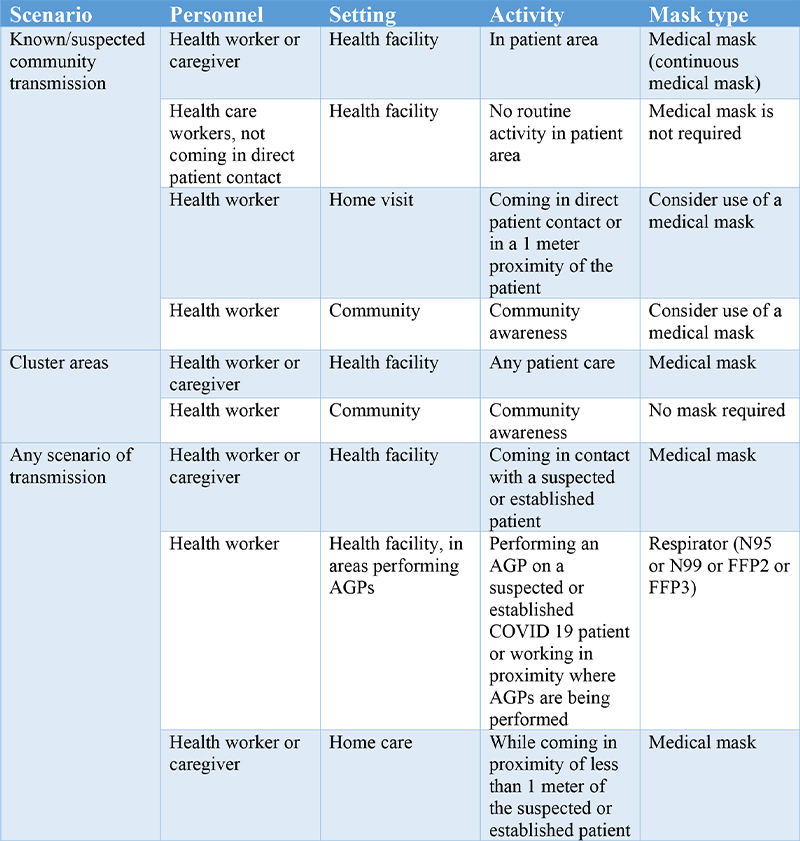
Guideline for using masks in the health care settings
A) Use of medical masks (surgical or procedure masks) and respirators (N95 masks) for caring suspected or confirmed COVID-19 patients



It is recommended that health workers who directly provide care or come in direct contact with COVID-19 patients, should wear a medical mask (along with other PPE components that are a part of aerosol and contact precautions), in the absence of aerosol-generating procedures (AGPs).
In areas where AGPs are being performed, it is recommended to health care personnel that they should wear a N95 or FFP2 or FFP3 or equivalent standard respirator.
B) Targeted continuous use of medical mask by health workers in locations of known or suspected COVID-19 community transmission.
In the context of areas, where community spread of COVID-19 is suspected or an intense COVID-19 outbreak exists, following recommendations are provided:
Health workers practicing in clinical area should always wear a medical mask during their routine activities throughout the entire shift; apart from the duration when they are having their meals and changing their medical mask after caring for a patient who requires droplet/contact precautions for other reasons
It is particularly vital to adopt the strategy of continuous use of masks in areas with a potentially higher risk of transmission such as triage, waiting lounges of family physicians or OPDs, designated COVID-19 hospitals, cancer units, transplant units etc.
While continuously using medical masks, it is also vital to:
- Change the mask if it gets wet, soiled or damaged.
- Not touch the mask to adjust it.
- If you have touched it, safely remove it, perform the hand hygiene procedure and use a fresh mask.
- Discard the mask and the PPE and use a new set after coming in contact with a patient for contact or droplet precautions.
- Personnel not working in clinical areas need not wear a medical mask during routine activities.
- PPEs including masks should not be shared between workers and be suitably disposed after use and not to be re-used.
- In addition to above recommendations, precautions of social distancing and hand hygiene practices should not be avoided as they are equally important.



Considerations for using non-medical masks
The utility of medical masks by the non-affected population may lead to a shortage of this extremely important supply to the health workers, who need them the most. In settings where medical masks are in short supply, medical masks should be reserved for use by only health workers and at-risk population when need arises.
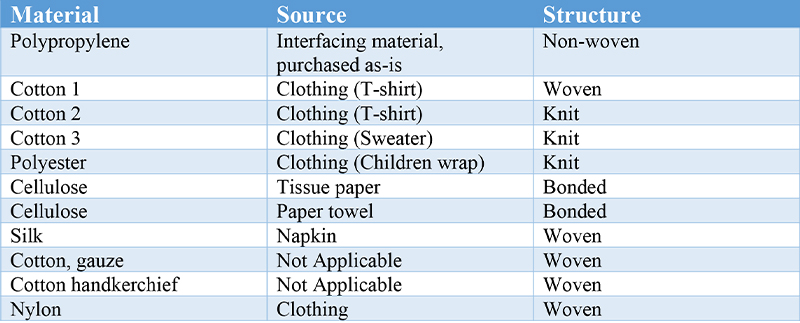
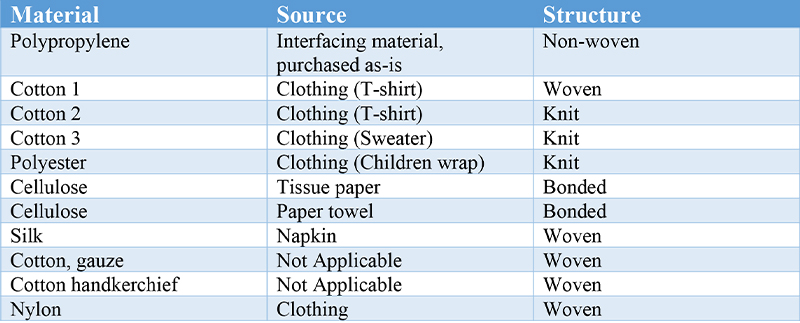
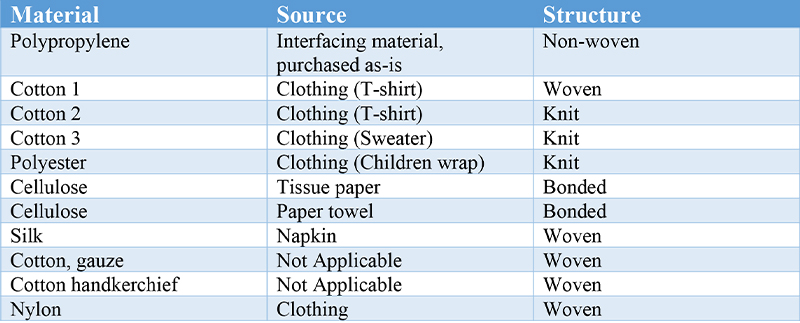
Non-medical or fabric masks are prepared from varied woven and non-woven fabrics like polypropylene. Non-medical masks may be composed from differing fabric compositions, sequences or layers and shapes. However, a non-medical mask is neither a medical or surgical device nor a PPE.
Usage Considerations
The use of non-medical masks, prepared from woven fabrics such as cloth, and/or non-woven fabrics, should only be considered for used by infected persons in unrestricted settings and not for prevention. They can be used temporarily for activities such as travelling on public transport when social distancing cannot be maintained, and their use should without fail go with frequent hand hygiene and physical distancing.
Elastic materials are not preferred to prepare masks as they get stretched after each use, causing increased pore size and lower effectiveness of the mask to filter droplets.
Layers
A minimum of three layers is needed for a non-medical mask, as per the used fabric. However, cotton handkerchief masks should consist of a minimum of 4 layers. Cotton gauze is found to be very porous with a filtration efficiency of only 3%.
The ideal material combination for non-medical masks should include three layers as follows: 1) an innermost layer of a material which absorbs water (e.g. cotton or cotton blends); 2) an outermost layer made of non-water absorbing material (e.g., polypropylene, polyester, or their blends) which may restrict external impurity from penetration through to the wearer’s nose and mouth; 3) a middle non-water absorbing layer of synthetic non-woven material such as polyproplylene or a cotton layer which may enhance filtration or retain droplets.
Shape
Shape of the non-medical mask should be flat-fold, fitting closely over the nose, cheeks and chin of the wearer. If the mask’s edges are not close to the face and shift, during activities like speaking, air penetrates through the mask’s edges rather than getting filtered through the fabric. The mask should be equipped to be held in place by the use of elastic bands or ties.
Coating
Coating the mask with materials like wax may raise the barrier and make the mask liquid-resistant, but too much coating may cause difficulty in breathing through the mask due to complete blocking of pores.
Maintenance
- Mask should be used only by a single person and not shared by multiple individuals
- All masks should be changed immediately, if they get wet or are visibly soiled
- When required, masks should be removed without touching the front portion of the mask and after mask removal, do not touch the eyes and mouth
- Discard the mask, if you wish or keep it in a sealable bag until you wash it. After washing, immediately perform hand hygiene
- Cloth masks should be frequently washed as per the cloth’s recommended washing temperatures
- Wash in warm hot water, 60°C, with soap or laundry detergent.
- Non-woven polypropylene (PP) may be washed at high temperatures, up to 125°C.
- Natural fibres may resist high temperature washes and ironing.
- Wash the mask delicately (without too much friction, stretching or wringing) if non-woven materials are used.
- The combination of non-woven PP and cotton can tolerate high temperatures; masks made of these combinations may be steamed or boiled.
- Where hot water is not available, wash mask with soap/detergent at room temperature water, followed by either i) boiling mask for one minute OR ii) soak mask in 0.1% chlorine for one minute then thoroughly rinse mask with room temperature water, to avoid any toxic residual of chlorine.
Wearing a face mask is not a substitute for physical distancing and basic hand hygiene but in some situations where you can’t follow social distancing and other preventive measures, wearing a mask can give you some layer of protection. It is important to follow the Government’s latest guidance on safeguarding yourself during the coronavirus pandemic, including travel advice within and outside the country.



